Medicaid Covers People with Pre-Existing Conditions, Too
Rachel Garfield and Robin Rudowitz
Published:
In recent weeks, the possible overturning of the Affordable Care Act (ACA) in court and the upcoming election have focused attention on the issue of protections for people with pre-existing conditions. Estimates of how many people have pre-existing conditions range from 54 million people with a declinable pre-existing condition—that is, a health condition that would have made them uninsurable in the pre-ACA individual insurance market—to over 100 million people with health conditions that could trigger other adverse actions such as higher premiums or coverage limitations. While the focus has been on the ACA’s private insurance protections, Medicaid also plays a significant role in covering people with pre-existing conditions.
Medicaid has always provided coverage for people with pre-existing conditions, even before the passage of the ACA. Prior to the ACA, individuals could be denied coverage in the private insurance market if they had a pre-existing condition. However, eligibility for Medicaid prior to the ACA was based on income and other categorical eligibility criteria (e.g., being parent or person with disability), not health status. If a person met these eligibility criteria, states could not deny Medicaid to that person even if he or she had a pre-existing condition. In addition, Medicaid coverage was explicitly extended over the years to several groups that do have pre-existing conditions, such as pregnancy or certain functional disabilities, for whom private insurers routinely used to deny individual insurance before the ACA. These protections were in place even before the ACA prohibited private health insurance discrimination based on health status and are part of the reason that Medicaid has historically covered many people with serious and persistent illnesses or disabilities (like HIV or serious mental illness) for whom private coverage was not available or if available, not adequate or too costly.
The expansion of Medicaid under the ACA extended Medicaid coverage to millions of adults who were previously ineligible for coverage without regard to pre-existing conditions. As of June 2019, 15 million adults were covered through the ACA eligibility pathway. If the ACA were overturned and federal matching funds were eliminated, it is likely that states would not retain eligibility for the vast majority of these people. While the majority of adult Medicaid enrollees work full or part-time, most are unlikely to have an affordable offer through their job and would face purchasing health insurance in an individual market where pre-ACA underwriting rules applied.
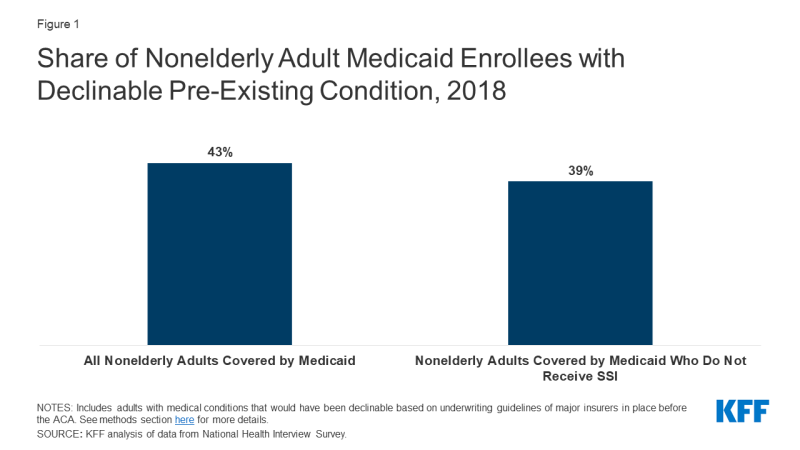
More than four in ten (43%) nonelderly adults with Medicaid had a declinable pre-existing condition in 2018 (Figure 1). Excluding the population that receives Supplemental Security Income and thus likely qualifies for Medicaid through a disability-related pathway, there are still nearly four in ten (39%) nonelderly adults with declinable pre-existing condition. Many of these adults likely gained Medicaid eligibility under the ACA expansion. If the ACA were repealed, both the Medicaid expansion and pre-existing condition protections would be overturned, leaving many of these adults likely uninsured.
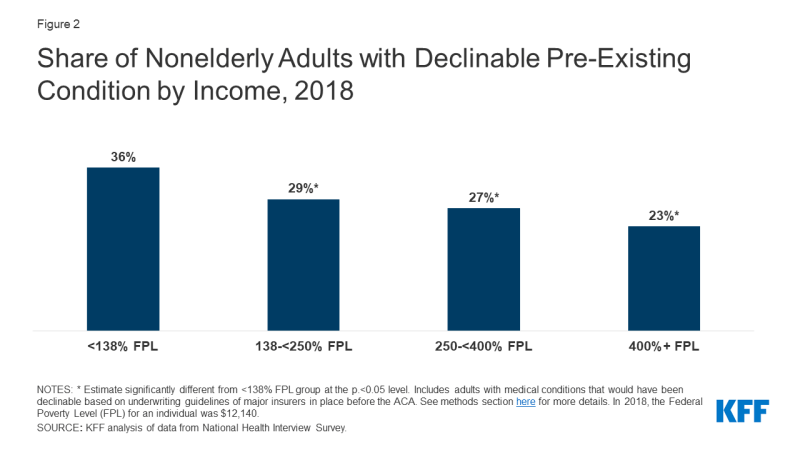
More broadly than Medicaid, adults with low incomes are more likely than those with higher incomes to have a pre-existing condition. More than one in three nonelderly adults with incomes below 138% of the poverty level – the threshold for expanded Medicaid eligibility under the ACA – have a pre-existing condition that would likely have led to a coverage denial before the ACA (Figure 2). Without the Medicaid expansion, availability of subsidies in the marketplace and protections for people with pre-existing conditions, most low-income people would not have options for affordable coverage and would likely be uninsured.