Racial Disparities in Flu Vaccination: Implications for COVID-19 Vaccination Efforts
Samantha Artiga, Josh Michaud, Jennifer Kates, and Kendal Orgera
Published:
With planning beginning for an eventual COVID-19 vaccine, one important consideration is making sure that distribution processes and outreach and communication strategies reach people of color. COVID-19 vaccination among people of color will be particularly important because they are bearing a heavy, disproportionate burden of the disease, and population immunity is not likely to be reached without high vaccination rates across all communities. However, doing so will require public health officials and providers to overcome a range of barriers to vaccination among people of color, many of which are rooted in a historic legacy of abuse and mistreatment by the medical system and ongoing racism and discrimination today.
Analysis of seasonal flu vaccination rates provides some insight into the potential barriers and issues to be addressed as part of COVID-19 vaccination efforts. Experts recommend an annual flu vaccination for all people age 6 months and older as the primary way to prevent sickness and death caused by the flu, and Healthy People 2030 national health objectives set a goal of vaccinating at least 70% of this population. Despite being widely recommended and fully covered as a preventive service under the Affordable Care Act (ACA), data show that overall flu vaccination rate remains low and that there are persistent racial disparities in uptake of the vaccine.
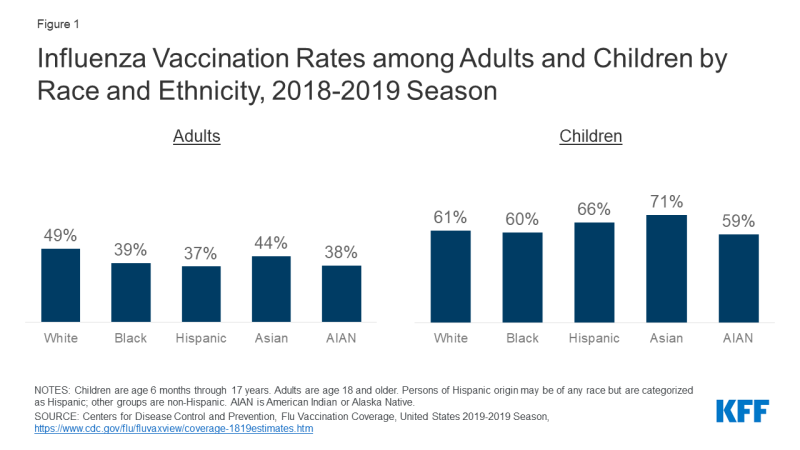
Analysis of flu vaccination rates shows persistent gaps and racial disparities in flu vaccination among adults. Data from the Centers for Disease Control and Prevention (CDC) show that the flu vaccination rate generally has been increasing over time but remains below the target level, with lower rates of vaccination among Black and Hispanic individuals compared to White individuals. These gaps and racial disparities in vaccination are concentrated among adults. During the 2018-2019 flu season, less than four in ten Black (39%), Hispanic (37%), and AIAN (38%) adults were vaccinated compared to nearly half of White adults (49%) (Figure 1). Vaccination rates were higher among children compared to adults and the rates for children of color were generally equal to or higher than those for White children.
The lower vaccination rates among adults of color, in part, reflect their higher uninsured rates. Data show that people of color are more likely be uninsured and less likely to have a usual source of care. Seasonal flu vaccines, especially for adults, are delivered and administered primarily through a system of private distributors and providers. As a preventive service under the ACA, the vaccine is available at no charge for individuals with insurance. However, uninsured individuals either need to pay out-of-pocket for the vaccine or identify sites, such as clinics or health centers, that are offering it for free. Evidence suggests that the federally-funded Vaccines for Children (VFC) program, which provides vaccines at no cost to children who might not otherwise be vaccinated because of inability to pay, has contributed to the higher vaccination rates among children across racial and ethnic groups. However, analysis of National Health Interview Survey data illustrates the barriers to vaccination facing uninsured adults. Across racial and ethnic groups, uninsured adults were less likely to be vaccinated compared to those with private coverage (Figure 2). Vaccination rates among adults with Medicaid coverage were similar to those with private coverage across most groups.
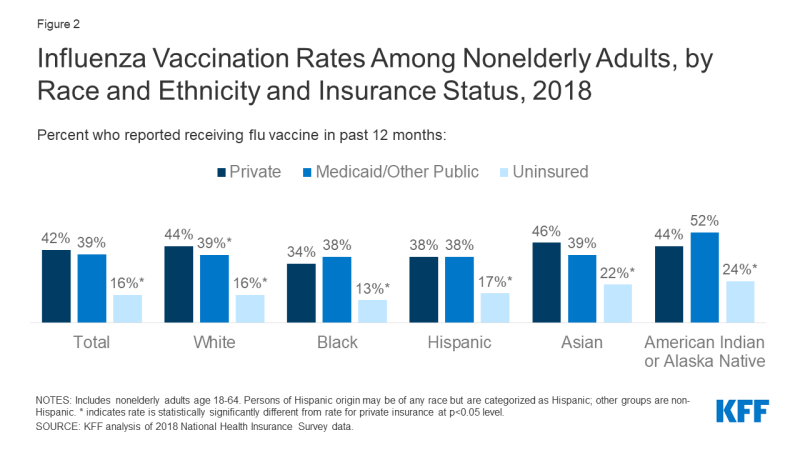
Figure 2: Influenza Vaccination Rates Among Nonelderly Adults, by Race and Ethnicity and Insurance Status, 2018
Research also shows that distrust, safety concerns, and experiences with discrimination and other factors contribute to disparities in vaccination rates. For example, research shows that, compared to White adults, African American adults perceive a higher risk of side effects from the seasonal flu vaccine, have less knowledge about the vaccine, and have less trust in the vaccine. Another study found that African Americans were more likely than any other group to cite concern over the vaccine causing influenza or serious side effects as the main reason for non-vaccination. Other research shows that African American and AIAN individuals were less likely than White individuals to say they believed the 2009 H1N1 influenza vaccine was “very safe.” Another study found that the majority of people would not accept a new but not yet fully approved vaccine, with Black individuals expressing the highest level of worry. Research also points to variation among Black individuals in willingness to obtain a vaccination, for example, finding that older adults were more likely to have attitudes that increase vaccine acceptance. Additional research finds that perceptions of racial fairness and the influence of race in health care settings as well as experiences with discrimination are associated with attitudes and beliefs about the flu vaccine that may influence willingness to obtain it. Beyond differences in beliefs and attitudes, other work suggests people of color may have more “missed opportunities” for flu vaccination, finding that adults of color were more likely to remain unvaccinated compared to White adults even when they had at least one health care visit during the flu season and indicated that they would be willing to get vaccinated if a healthcare provider strongly recommended it.
Together these findings show that once a COVID-19 vaccine becomes available, accomplishing a high vaccination rate will require addressing multiple barriers to vaccination among people of color, including access-related challenges and distrust and safety concerns. Under federal law, insurers must make the COVID-19 vaccine available at no cost. The Trump administration has also indicated it will make the vaccine available to uninsured individuals at no cost, but questions remain about whether there is sufficient funding to cover these costs. Beyond addressing cost barriers, it also will be important to make the vaccine easily accessible at convenient locations and to ensure people know where and how to access it free of charge. Moreover, effective outreach and media strategies will be important to build public trust and willingness to get the vaccine. People of color’s distrust of the health care system, particularly among Black individuals, reflects the historical legacy of the system’s abuse and mistreatment of people of color and ongoing racism and discrimination today. Distrust and safety concerns are likely to be further compounded in the context of COVID-19 vaccination efforts since the majority of the public is concerned that political pressure from the Trump administration will lead the Food and Drug Administration to rush to approve a vaccine without making sure that it is safe and effective. Research suggests that health care providers and public health agencies can increase education about vaccine recommendations and that health care providers can increase vaccine acceptance by recommending and offering a vaccine at the same time. Previous public health and health coverage enrollment experience further points to the importance of providing information in linguistically and culturally appropriate ways, proactively addressing people’s concerns, and using trusted individuals from the community as messengers. Even with targeted strategies, it likely will be difficult to overcome distrust and safety concerns, further amplifying the importance of using trusted messengers to share information and conduct outreach to the community.