
The independent source for health policy research, polling, and news.
Costly GLP-1 Drugs are Rarely Covered for Weight Loss by Marketplace Plans
For Drugs Used to Treat Diabetes, Plans Almost Always Require Prior Authorization or Other Utilization Management
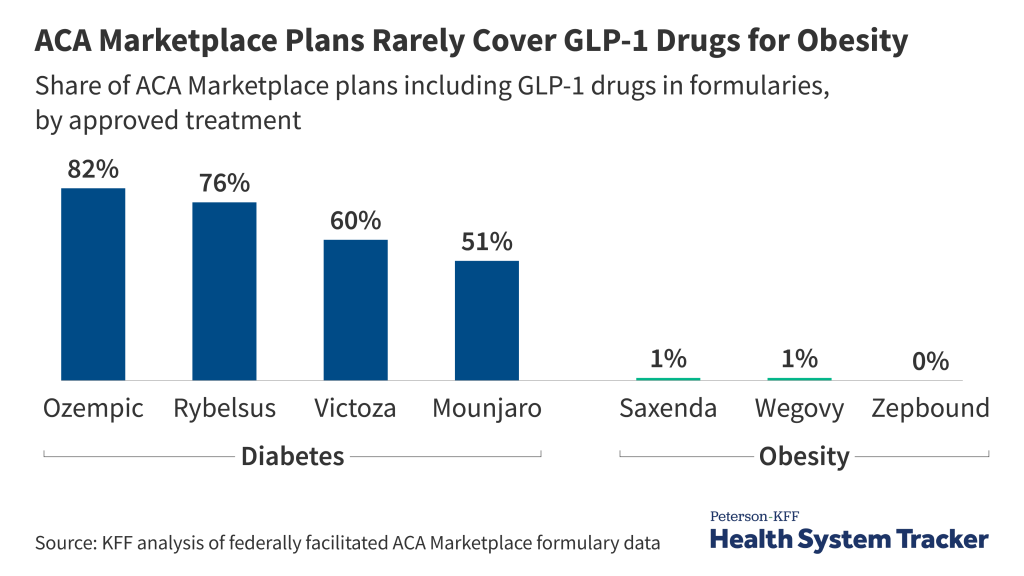
Affordable Care Act (ACA) Marketplace plans rarely cover GLP-1 drugs approved solely for obesity treatment, according to a new KFF analysis of 2024 federal plan data. Wegovy, a drug that is approved for weight loss, is covered by just 1% of Marketplace prescription drug plans, compared to 82% of Marketplace prescription drug plans for Ozempic, which contains the same active ingredient as Wegovy (semaglutide) but is approved only for diabetes.
When GLP-1 drugs are covered for diabetes treatment, almost all plans use at least one utilization management strategy to control costs, such as prior authorization or quantity limits. Of the few Marketplace plans that cover GLP-1 drugs approved for obesity, all require prior authorization.
Utilization management tools are intended to balance cost control and access but may still pose barriers for people with a medical necessity to take these drugs. While insurers receive rebates to offset some of their costs, the list prices of GLP-1 drugs are about $1,000 per month, and growing demand for these medications could put upward pressure on premiums.
This analysis examines publicly available formularies of plans available on the federally facilitated ACA Marketplaces in 2024 and does not include states that run their own Marketplaces, where coverage patterns may differ. The ACA Marketplaces represent a small share of people with private health insurance, as most people with private coverage have plans sponsored by their employers. While information on employer plan formularies is not publicly available, these plans may be more likely to cover drugs for weight loss than ACA Marketplace plans given the desire to attract workers, though they may employ similar utilization management strategies.