Telemedicine in Sexual and Reproductive Health
| Key Takeaways |
|
Introduction
The World Health Organization (WHO) defines telemedicine as the provision of health care services by health care professionals, utilizing technology to exchange information in the diagnosis, treatment and prevention of disease. While not yet broadly adopted across the U.S., telemedicine’s use in reproductive health care has shown promise in offering innovative solutions to unmet health needs, particularly in areas with few health care providers. Leading medical groups endorse telemedicine in bolstering reproductive health services and expanding access for rural women. This brief presents an overview of telemedicine’s current use in sexual and reproductive health care, and reviews considerations in its coverage, potential to improve access, and financial implications for providers and patients.
Telemedicine Background
Varied definitions for telemedicine and telehealth exist. In the broadest definition, telemedicine can include basic telecommunication tools like phone calls, text messages, emails, faxes and online patient health portals that allow patients to schedule appointments, read appointment summaries, view lab results and communicate with their providers. Many health care organizations and insurers, however, adopt a narrower definition, typically involving three specific telemedicine modalities:
- Videoconference: real-time exchange of information via video. Example: patient has an appointment on a web-based platform with a clinician.
- Store and forward: an online consultation in which patient information is sent to a remote clinician, who later sends back diagnostic/treatment recommendations.
- Remote patient monitoring: patient’s home monitoring device sends data to clinician for review. Example: home blood sugar data sent to doctor remotely.
Telemedicine facilitates remote interactions between patients and providers or between providers of different specialties, originating from health care facilities or a patient’s home (Figure 1). A patient may see their usual provider during a telemedicine visit, remaining within their existing health care system, or may interact with remote providers they have never met before, for example on a third party application.
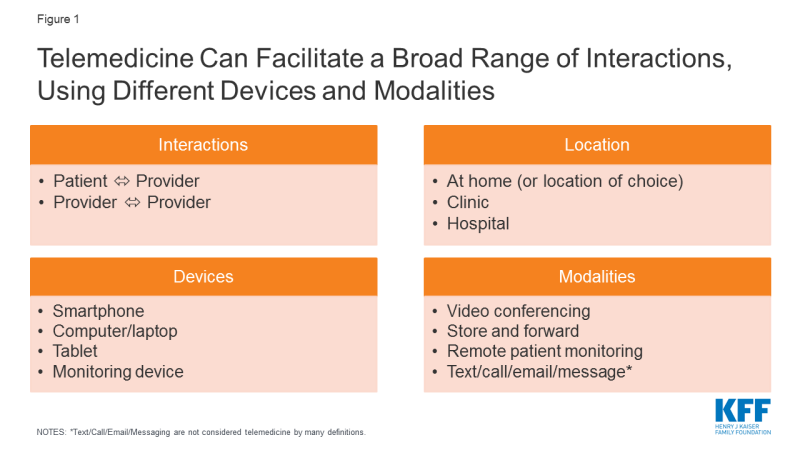
Figure 1: Telemedicine Can Facilitate a Broad Range of Interactions, Using Different Devices and Modalities
Due to its diverse functions, telemedicine has long been touted as a method to increase health care access, focused on rural populations where clinicians are scarce. KFF’s 2017 Women’s Health Survey revealed many women, particularly low-income women, delay or forgo necessary health care due to problems obtaining transportation or childcare, indicating that telemedicine could be beneficial in low-income, urban populations as well.
Despite its potential, patient use of telemedicine appears small. An analysis of private insurance claims by FAIR Health reveals telemedicine use grew 14-fold for non-hospital patient-provider interactions from 2014-2018, but still represented only a small fraction of all medical claims (0.1%). Urban areas experienced more growth than rural, and the majority of utilizers were women (65%) and ages 31-40 (21%). Patients may be reluctant to adopt telemedicine, preferring in-person visits to videoconferencing, and establishing rapport via video poses challenges to patient engagement. In a study of health care consumers, 43% of respondents thought telehealth visits would be less personal than traditional services, and 49% perceived the quality of care to be lower. Since users may engage with different providers each time they utilize telemedicine, continuity of care may be disrupted as well.
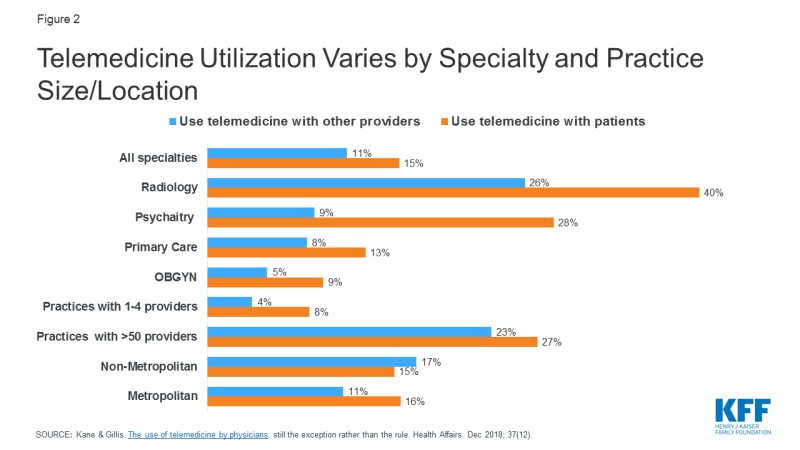
Among providers, a 2016 survey of physicians found just 15% of physicians worked in practices offering telemedicine services, with primary care providers and OBGYNs using telemedicine considerably less than specialties like radiology and psychiatry (Figure 2). Uptake for telemedicine was notably higher among larger practices, and in non-metropolitan areas for provider to provider interactions.
Reproductive Health Services in Telemedicine
A broad range of gynecologic and obstetric services can be offered via telemedicine, including contraception, medication abortions, STI care, prenatal care, and limited applications in OB-Psychiatry, men’s sexual health and care for sexual assault victims (Table 1). The modalities of delivery and levels of patient-provider interaction vary across these services.
| Table 1: Scope of Reproductive Health Services in U.S. Offered via Telemedicine | ||
| Services available | Example platforms/providers | |
| Contraception | Hormonal contraception: oral contraceptive pills, vaginal ring, patch | Alpha Medical, Hers, HeyDoctor, Lemonaid, Maven, Nurx, Pandia Health, Planned Parenthood Direct, Plushcare, PRJKT Ruby, the Pill Club, Simple Health, Twentyeight Health, Virtuwell |
| Emergency contraception | Maven, Nurx, Pandia Health, PRJKT RUBY, The Pill Club, Virtuwell | |
| Abortion | Medication abortion | Planned Parenthood, TelAbortion |
| STI Care | STI testing (mail in self-collected samples vs. in-lab testing) | Binx Health, I Want the Kit, Let’s Get Checked, myLAB box, Nurx, Everlywell, CheckMate, PersonaLabs, STD check, PlushCare, Virtuwell, Roman. |
| Treatment for select STIs | ||
| PrEP for HIV prevention | PlushCare, Nurx | |
| At-home HPV testing | Nurx, Binx Health | |
| Telemedicine assisted colposcopy | Select research studies | |
| Prenatal Care | Prenatal care for low- and high-risk pregnancies | University of Arkansas for Medical Sciences (UAMS), Mayo Clinic, University of Utah, George Washington University (GWU) |
| At-home monitoring: blood pressure, fetal heart rate, fundal height, blood sugar | UAMS, Mayo Clinic, BabyScripts (partnering with GWU, Penn Medicine, MedStar Health, UTHealth, Medical University of South Carolina, etc.) | |
| Video consultation with specialists | University of Pittsburgh | |
| Obstetrics & Mental Health | Prenatal OB-Psych care | University of Arkansas for Medical Sciences (UAMS) |
| Postpartum depression care | Chiron Health, Amwell | |
| Men’s Sexual Health | Treatment for erectile dysfunction, premature ejaculation | Roman |
| Sexual Assault | Video consultation with forensic sexual assault nurse examiners | Penn State SAFE-T center |
KFF Analysis of Outpatient Telemedicine Utilization in Reproductive Health Care
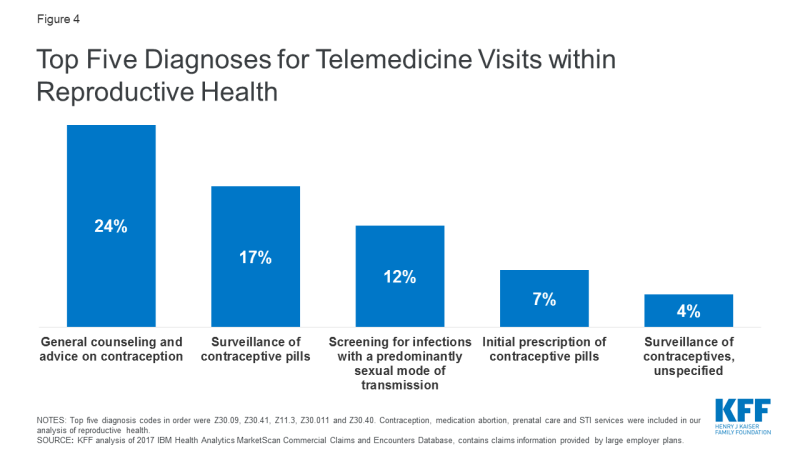
Use of telemedicine in reproductive health care is minimal. KFF analyzed outpatient telemedicine utilization among individuals with large employer sponsored health plans, using the 2017 IBM Health Analytics MarketScan Commercial Claims and Encounters Database. 51,758,413 weighted claims were analyzed within the reproductive health categories of contraceptive management, medication abortion, prenatal care, and STI testing and treatment. 11,089 of these claims were delivered via telemedicine, meaning telemedicine services accounted for just 0.02% of all reproductive health claims.1 Within telemedicine claims for reproductive health, visits for contraceptive management were the most common (65%), followed by prenatal care (21%) and STI services (17%). Use of telemedicine for medication abortion was minimal (<1%) (Figure 3). The most frequent reproductive health diagnosis codes for telemedicine claims are shown in Figure 4. These data do not capture use of telemedicine on platforms that do not accept private insurance, or by patients with public insurance or no insurance.
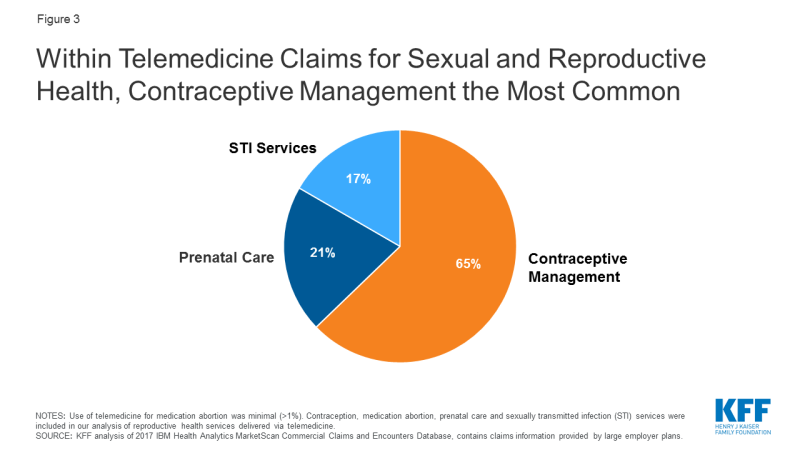
Figure 3: Within Telemedicine Claims for Sexual and Reproductive Health, Contraceptive Management the Most Common
Contraception
The most effective forms of birth control, including long acting reversible contraceptives (LARCs), require in-person care, but providers can prescribe a variety of other contraceptive methods via telemedicine, including oral contraceptive pills (OCPs), the patch and vaginal ring. As of June 2019, 14 online OCP platforms existed in the U.S. All determine eligibility and prescribe OCPs in the same general manner:
- Using a smartphone or computer, the patient provides a health history via a questionnaire or video consultation with a clinician.
- The clinician reviews the information remotely and determines eligibility for OCPs. The provider may be a doctor, nurse practitioner, physician assistant or certified nurse midwife, often depending on state law.
- The patient receives the OCPs by pharmacy pick-up or mail. Prescriptions are valid for 3-12 months, with a 1-12 month supply at a time, depending on the platform and insurance provider.
Almost all risk factors precluding use of hormonal birth control can be assessed online; evaluations screen for age, smoking history, and conditions posing significant health risks including clotting disorders, heart disease, breast cancer, and migraines with aura. These platforms cannot measure blood pressure, typically a necessity before initiating OCPs, but most require the user input a reading from the last year; the CDC deems this method acceptable if a provider cannot measure the blood pressure.2 A study of 9 telecontraception platforms found OCPs were prescribed when contraindicated in 3 of 45 visits, but adherence to CDC Medical Eligibility Criteria actually may be higher than for in-person visits. This suggests telemedicine prescription of OCPs is safe, as compared to traditional care.
Select platforms offer emergency contraception (Table 1). While levonorgestrel (LNG)/Plan B One Step can be accessed over the counter, ulipristal acetate (UPA)/Ella, requires a prescription. UPA is more effective in preventing pregnancy than LNG, especially for overweight and obese individuals, and can be taken up to 120 hours after unprotected sex (LNG has a 72 hour limit). Telemedicine prescription of UPA could allow for quicker and broader access to this medication.
Cost and coverage
Out of pocket costs for OCPs via telemedicine includes the consult fee, contraceptive product and delivery fee. Across the available platforms, a patient can expect to pay anywhere from $0 to more than $170 for the OCP prescription and a 1 month supply. This can total an average $313 per year (range $67to $519) for an uninsured patient according to a recent study. Many platforms accept private insurance to cover the cost of the contraceptive product, but not necessarily the consult or delivery fee. Some platforms do not accept any insurance plans, and almost none accept Medicaid (Table 2). Limited information is available on the cost of other types of contraception (patch, ring).
Under the ACA, most private insurance plans are required to cover FDA-approved contraceptive services and supplies without cost-sharing to the patient, but the providers must be in-network which is not always the case for telemedicine. Medicaid programs are similarly required to cover family planning services without cost-sharing to the patient, but because many platforms do not accept insurance, particularly public insurance, insurers may not reimburse patients for these applications. Therefore, telemedicine users pay more for contraception out of pocket than those who have an in-person visit with an in-network provider, which most plans are required to cover in full.
| Table 2: Estimated Out of Pocket Costs for Oral Contraceptive Pills Prescribed via Telemedicine | ||||
| Consult Fee | Contraceptive Product | Delivery Fee | Total | |
| Out of Pocket Cost | $0-99 | $0-30/month | $0-49 | $0-178 (1 month supply) |
| Platform accepts private insurance for: | Varies by platform | Typically yes | Typically no | $0-178 (1 month supply) |
| Platform accepts Medicaid for: | Typically no | Varies by platform | Typically no | $0-178 (1 month supply) |
| SOURCE: Free the Pill Prescribing Resources 2019; Zuniga et al. 2019. | ||||
Access and policy
OCPs via telemedicine are available in all 50 states, D.C., Puerto Rico and the U.S. Virgin Islands, from at least two vendors per state. That said, most telemedicine platforms only operate in specific states, likely due to challenges expanding across state lines. For example, TwentyEight Health only prescribes to NY and NJ residents, while PRJKT RUBY is available in 49 states and Planned Parenthood Direct will operate in all 50 states by the end of 2020.
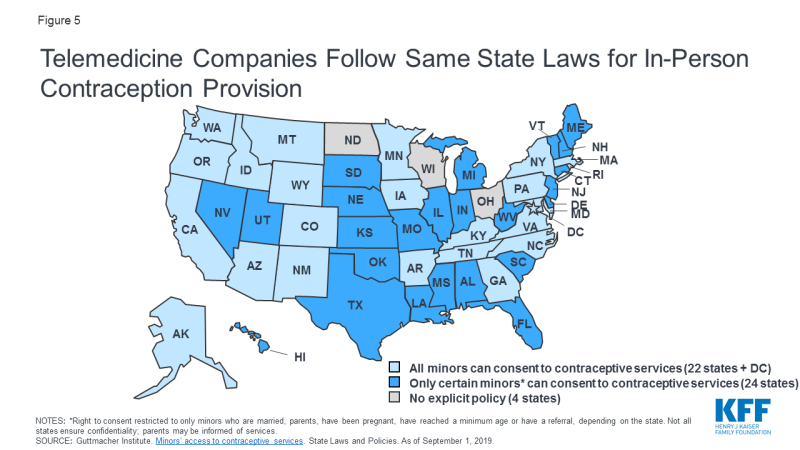
To date, no policies specifically prohibit the use of telemedicine for contraception. Rather, telemedicine services for contraception follow the same state laws as do in-person services. For example, many telemedicine platforms for contraception have an 18+ age requirement, often in accordance with state laws (Figure 5). Several platforms also impose upper age limits, typically from 35-50 years old, likely due to safety concerns.
Abortion
Medication abortions use medications to terminate pregnancy, most commonly mifepristone and misoprostol. Medication abortions are FDA approved until 10 weeks gestation, are highly safe and effective and account for approximately 39% of all abortions. Due to the myriad of restrictions on abortion, many communities do have not have access to medication abortion, and even in places where it is available, some states require patients have at least two visits to obtain the pills.
| Table 3: Delivery Models for Telemedicine Medication Abortion | ||||
| Model | Example | Description | Availability | Safety & Efficacy |
| Site-to-site | Planned Parenthood (PP) | 1. Patient goes to participating PP clinic for intake appointment and ultrasound.
2. Remote PP provider reviews history and imaging. If eligible, provider remotely unlocks medication drawer in patient’s room. 3. Patient takes mifepristone in clinic, misoprostol at home. 4. Patient returns to clinic in 2 weeks. |
14 states[3] | Highly safe and effective in the termination of pregnancy, with high patient satisfaction (Kohn et al. 2019, Grossman et al. 2011, Grossman and Grindlay 2017). |
| Direct-to-Patient | TelAbortion FDA-approved clinical trial | 1. Patient goes to any nearby clinic for pre-treatment labs and ultrasound.
2. Patient sends results to TelAbortion study, provider determines eligibility. 3. If eligible, patient mailed medications. 4. Follow up via phone or videoconference. |
8 states: CO, GA, HI, ME, NM, NY, OR, WA | Found to be safe, feasible and acceptable to patients (Raymond et al. 2019). |
| Fully Remote | Women on Web | 1. Patient fills out online questionnaire.
2. Provider remotely reviews info. 3. If eligible, patient receives medications by mail. Process may require in-person visits if determined to need ultrasound or RhoGAM. |
Not available in U.S. | Studies in Ireland and across 33 countries finds method is effective, low rates of adverse events (Aiken et al. 2017, Gomperts et al. 2008). May increase surgical intervention risk (Gomperts et al. 2014). |
To address limited access, Planned Parenthood pioneered the first telemedicine medication abortions in the U.S. in 2008. Their protocol is classified as a “site-to-site” model, whereby a clinician remotely prescribes medication abortions by collaborating with Planned Parenthood centers that do not have on-site abortion providers; the patient receives their labs, ultrasound and medications all from their local Planned Parenthood clinic (Table 3). Alternatively, the TelAbortion study, a FDA-approved clinical trial run by Gynuity Health Projects, uses a “direct-to-patient” model. In this model the patient consults with a remote clinician, obtains labs and an ultrasound from any nearby clinic, and if deemed eligible, receives their medications by mail. While in-person services are still required, the difference between this and “site-to-site” is the freedom for patients to obtain pre-treatment tests from any convenient medical facility, rather than only partnering sites. Both the TelAbortion and the Planned Parenthood protocols have been shown to be safe, effective and acceptable to patients when compared to in-person care, but are only available in certain states.
Efforts are underway to provide telemedicine abortions without ever visiting a health care facility. In this “fully remote” model, the patient completes an online questionnaire to assess (1) confirmation of pregnancy, (2) gestational age and (3) blood type. If determined eligible by a remote clinician, the patient is mailed the medications. This model does not require an ultrasound for pregnancy dating if the patient has regular periods and is sure of the date of their last menstrual period (in line with ACOG’s guidelines for pregnancy dating). If the patient has irregular periods or is unsure how long they have been pregnant, they must obtain an ultrasound to confirm gestational age and rule out an ectopic pregnancy3 and send in the images for review before receiving their medications. If the patient does not know their blood type or has Rh negative blood, the provider may prompt the patient to visit a nearby clinic for an injection to prevent adverse reactions between maternal and fetal blood (RhoGAM), if indicated.
Women on Web successfully implements this model in multiple countries outside of the U.S. Multiple studies find their service is safe and effective, but may lead to small increased need for surgical intervention. AidAccess started offering this model in the U.S, using a remote physician in Europe and a pharmacy in India. This delivery system blends into the concept of “at-home” or “self-managed” abortions, however in telemedicine abortions, a clinician is always involved in the safe prescribing of these medications. The FDA issued a cease and desist letter to AidAccess as this service is not currently legal in the U.S.
Cost and coverage
Cost estimates for telemedicine abortions are not readily found. Per TelAbortion’s website, costs will depend on the patient’s state, required tests and insurance coverage, but the study will provide a cost estimate before enrolling. Similarly, patients must call their nearest Planned Parenthood for telemedicine abortion cost estimates. For in-person care, the Turnaway study found the average out of pocket cost to be $461 for a first trimester medication abortion across 30 U.S. sites; women also spent from $0 to $2200 (mean of $54) on related travel costs. Telemedicine abortions may cost similar to those in-person, but patients may save on transportation, childcare and lost wages.
Insurance coverage for abortion can be limited. The Hyde Amendment prohibits use of federal funds for abortion except in cases of rape, incest or endangerment to the woman’s life. This limits abortion funding for Medicaid enrollees, federal employees, and those covered by the military, Veterans Affairs, and Indian Health Service. In addition, several states restrict abortion coverage in private insurance plans (though most people with employer-provided health coverage are in self-insured plans, outside the reach of state restrictions). This means many people who obtain abortions incur out of pocket fees, regardless of their insurance plan. Should telemedicine abortions become more widely available, these limitations would apply.
Access and policy
Telemedicine services must abide by the same regulations as those for equivalent in-person services. Therefore, the multitude of laws enforced for in-person abortion services, including physician and hospital requirements, gestational limits, waiting periods, and age restrictions, all apply to telemedicine abortions. Telemedicine abortions are then subject to additional prescribing barriers described below.
Prescribing Barriers
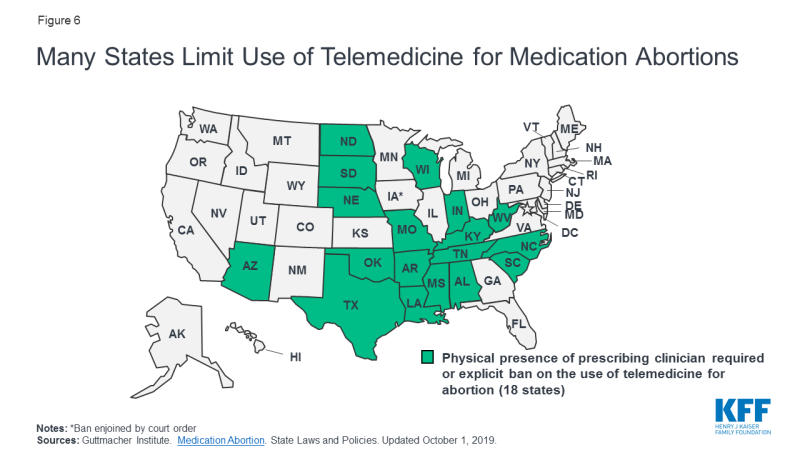
A few states explicitly prohibit use of telemedicine in abortions (AZ, KY), while 18 states require the prescribing clinician be physically present with the patient for a medication abortion. This effectively prohibits all telemedicine abortions in those states (Figure 6). Indiana also prohibits prescription of medication abortions if the prescriber has not previously examined the patient in-person.
Telemedicine abortions are further limited by the FDA Risk Evaluation and Mitigation Strategy (REMS) on mifepristone, despite its exceedingly low rate of adverse events. Mifepristone’s REMS means it may only be dispensed by certified providers in clinics and hospitals, and is not available in commercial pharmacies or by mail like most other medications. The REMS also requires a prescriber and a patient agreement form before dispensing the medication, complicating remote provision of abortions. TelAbortion obtained a FDA waiver for their telemedicine study, allowing them to mail mifepristone directly to patients which is normally prohibited. If the REMS for mifepristone were lifted, the availability of medication abortions by telemedicine would likely increase.
What is a Risk Evaluation and Mitigation Strategy (REMS)? A REMS creates a strategy for medication prescribing, typically to decrease adverse events for drugs with safety concerns. 59 drugs currently require a REMS due to their life-threatening side effects, including several opioids, antipsychotics and cancer treatments. Mifepristone is associated with low rates of adverse events, and many urge for its REMS to be removed.
Scope of Practice
While not specific to telemedicine, 34 states only allow licensed physicians to prescribe medication abortions, excluding advanced practice clinicians (APCs) like nurse practitioners, certified nurse midwives and physicians assistants. For APCs trained in abortion care, multiple studies show their skills are safe and comparable to those of physicians. By reducing the number of providers allowed to offer abortions, the use of telemedicine abortion is indirectly limited.
STI Care
Several mobile apps and online services provide STI consultation, testing and treatment (Table 4). Most allow users to select a testing panel, which they then obtain through in-person lab centers like Quest or LabCorp. Some platforms offer at-home collection kits, where the consumer mails in self-collected samples to a lab for testing; this could involve self-collection of urine, a vaginal, rectal or oral swab or a finger prick blood sample. For positive results, several platforms offer provider consultation and prescribe treatment for select STIs (typically gonorrhea, chlamydia, trichomonas and herpes), with medications shipped home or ordered to a pharmacy. For some positive results, however, including HIV and syphilis, users would be prompted to seek in-person care for an exam and additional testing. Telemedicine STI testing may be ideal for individuals who are asymptomatic but may have been exposed to a STI after unprotected sex, but if the patient is showing symptoms, an in-person exam is still typically needed. Select platforms do not require testing before STI treatment, particularly for expedited partner therapy or acute flares of known herpes infections, and others prescribe PrEP (pre-exposure prophylaxis) for the prevention of HIV. Most platforms offer care to all genders, but Roman specializes in men’s sexual health.
Telemedicine has also been used to evaluate risk for cervical cancer. Nurx and Binx Health offer at-home HPV screening, to test for the strains of HPV that cause genital warts and cervical cancer; patients still require in-person pap smears to check the cervix for cancerous or pre-cancerous cells. For women with abnormal pap smears who need colposcopies, one study trialed transmitting live images of the cervix to a remote provider to determine the need for a biopsy or further testing. This study was limited by low quality images, and resulted in additional testing for patients.
Telemedicine care may be appealing to individuals who do not feel comfortable seeking in-person STI care due to stigma or privacy concerns; that said, not all mobile apps comply with the Health Insurance Portability and Accountability Act (HIPAA). Some consumers may doubt their ability to self-collect samples for testing, but studies show this collection method is feasible and acceptable to most patients, may increase uptake of testing by patients, and yields test results comparable in accuracy to clinician-collected samples for HPV, trichomonas, gonorrhea and chlamydia. The only FDA approved at-home HIV test requires the user collect an oral swab, test the sample and read the results at home; studies reveal false negative results are more common than for in-clinic testing using this method. More often however, telemedicine platforms have users mail in self-collected samples to a lab; the accuracy of this method compared to in-clinic testing remains unclear. False negatives may also occur if users order tests too soon after unprotected sex. To ensure quality results, users should look for platforms using FDA approved tests and labs accredited by the College of American Pathologists (CAP) and certified under the Clinical Laboratory Improvement Amendments (CLIA).
| Table 4: Examples of STI Services Available via Telemedicine | ||||
| Company | Services Offered | Cost and insurance | Availability | Accuracy & Privacy |
| Binx Health | At-home testing
Select treatment |
No insurance accepted.
STI testing: $69 to $425* |
All states except NJ, NY, RI | CAP + CLIA certified labs.
HIPAA compliant platform. |
| I Want The Kit: Johns Hopkins | At-home testing
Select treatment |
Collection kit + lab testing: $0
Return postage: $3.66 for DC. Fees may apply for treatment. |
AK, DC, MD | CAP + CLIA certified labs.
HIPAA compliant platform. |
| Let’s Get Checked | At-home testing
If positive, phone consult + treatment |
No insurance accepted.
STI testing: $99-269* |
All states except NJ, MD, RI | CAP + CLIA certified labs.
HIPAA compliant platform. |
| myLAB Box | At-home testing
If positive, phone consult |
Accept FSA/HSA cards
STI testing: $79-369* |
All states | CAP + CLIA certified labs.
HIPAA compliant platform. |
| PersonaLabs | In-lab testing. If positive, provider consult + treatment. | Accept FSA/HSA cards
STI testing: $46-522* Consult: $70-125 |
All states except NY, NJ, RI | CLIA certified labs.
HIPAA compliant platform. |
| STD check | In-lab testing
Select treatment |
No insurance accepted.
STI testing: $24-349* |
4,500 test centers | CLIA certified labs.
HIPAA compliant platform. |
| Everlywell | At-home testing
Phone consult Select treatment |
No insurance accepted.
STI testing: $69-199* Phone consult: $0 w/ testing |
Testing: 50 states. Treatment: 46 states | CLIA certified labs.
Use ClearData to host data (HIPAA compliant) |
| Nurx | At-home testing
PrEP prescriptions |
Accepts private insurance.
Consult: $12. Shipping: $15 STI testing: $75 w/ insurance, $160-220* w/out insurance. |
26 states | CAP + CLIA certified labs.
HIPAA compliant platform. |
| CheckMate | At-home or in-lab testing. If positive, consult + treatment. | No insurance accepted.
STI testing: $63-269* Consult: $0 if test positive |
Unable to obtain information | CAP + CLIA certified labs.
HIPAA compliant platform. |
| PlushCare | In-lab testing
Select treatment PrEP prescriptions |
Accepts private insurance.
“Sexual Health” testing: $199 Consult: $99 w/out insurance. |
All 50 states and D.C. | Labs: LabCorp + Quest Diagnostics.
HIPAA compliant platform. |
| NOTES: This is not an exhaustive list of all telemedicine platforms offering STI care. *The cost of STI testing panels varies based on the number of type of tests ordered. Abbreviations: CLIA: Clinical Laboratory Improvement Act. CAP: College of American Pathologists. HIPAA: Health Insurance Portability and Accountability Act |
||||
Cost and coverage
STI care via telemedicine can come with significant out of pocket costs to the patient (Table 4). While some platforms accept private insurance, most do not accept Medicaid, and many do not accept any insurance plans. Scant data exists comparing out of pocket costs for STI care using telemedicine to in-person care, however for most patients, telemedicine could cost more; this is because the ACA requires most private insurance plans and states with Medicaid expansion to cover recommended STI counseling and screening at no cost sharing to the patient. By 2021, state Medicaid programs and most private insurances will be required to cover the cost of PrEP for individuals at risk for HIV with no patient cost-sharing. For uninsured patients, STI services are often covered at no or low cost at publicly funded STI clinics, while these individuals would pay full price for telemedicine services. That said, insured individuals may not use their coverage to pay for STI care; in a study of U.S. STD clinics, 62% of patients with private insurance, 65% of patients on their parent’s insurance and 37% of patients on Medicaid were not willing to use their insurance for their visit, opting to pay out of pocket presumably due to privacy concerns. Individuals may be willing to pay more out of pocket for telemedicine in exchange for greater anonymity and forgoing in-person interactions.
Access and policy
Some telemedicine platforms for STIs operate in all 50 states, whereas others are restricted to certain regions (Table 4). Most platforms place age restrictions on its users; for example you must be ≥13 years old to access STI testing through Nurx and ≥18 for PlushCare. These limits are often more restrictive than state laws regarding minors and STI care; as of August 2019, minors in all 50 states and DC can consent to STI services, although 11 states require a minimum age (typically 12-14 years old). Most states do not mention STI care in their telemedicine reimbursement laws, but select states do. For example Texas and New Mexico specifically do not require in-person evaluation before expedited partner therapy, allowing telemedicine’s use for these cases.
Crosscutting Issues
State Regulation
All 50 states and D.C. define, regulate and reimburse for telemedicine differently. According to the Center for Connected Health Policy’s (CCHP) report on state telehealth laws, in 2018 over 160 telemedicine related bills were introduced, reflecting the field’s ever-changing policy landscape. This complexity creates challenges for patients in knowing what services are covered, and for providers who must ensure they comply with evolving state laws. Below we outline key issues related to the regulation and reimbursement of telemedicine. For the most up to date information, CCHP provides an interactive tracking tool for state and federal legislation regarding telehealth policy.
Licensing and Malpractice
Clinicians must be licensed to practice in states where they offer telemedicine services. For example, if a clinician is located in CA, but is providing services remotely to a patient in MA via telemedicine, the provider must be licensed in MA, the state where the patient is located. Nine states require special licenses specific to telemedicine (AL, LA, ME, NV, NM, OH, OR, TN, TX). Others participate in “compacts” that allow providers in participating states an expedited process to practice in other compact states. As of October 2019, 34 states participate in the enhanced Nurses Licensing Compact, and 29 states and D.C. participate in the Physician’s Interstate Medical Licensure Compact. Clinicians must also ensure their malpractice insurance covers telemedicine and services provided across state lines. Insurance premiums may be higher if covering telemedicine, and Hawaii is the only state to require malpractice carriers to offer telemedicine coverage.
Online prescribing
Most states require a patient-provider relationship be established before e-prescribing of medications. Many telemedicine platforms use an online health questionnaire to establish that relationship, but in at least 15 states, this method is considered inadequate (AR, CO, DE, FL, HI, ID, IA, KS, KY, LA, ME, MO, NM, WA, WI). Instead, a physical exam would be required before prescribing, either in-person, by live-video, or by a referring physician, depending on the state. Therefore, in certain states an app prescribing OCPs may need to establish the patient-provider relationship via live-video, rather than a questionnaire. Examples of online prescribing laws addressing telemedicine are shown below (Table 5).
| Table 5: Examples of State Laws Addressing Prescribing Medications via Telemedicine | |
| State | Law Description |
| AZ | The physical or mental health status exam can be conducted during a real-time telemedicine encounter. |
| AR | A patient completing a medical history online and forwarding it to a physician is not sufficient to establish the relationship, nor does it qualify as store-and-forward technology. |
| CO | Pharmacists are prohibited from dispensing prescription drugs on the basis of an internet-based questionnaire or a telephone consultation, without a valid pre-existing patient-practitioner relationship. |
| ND | An e-prescription can be issued via telemedicine if the referring provider conducted an in-person exam. |
| WV | Prohibits providers from issuing prescriptions without establishing an ongoing physician-patient relationship (exceptions apply). |
| NOTES: This table highlights common regulations but it not an exhaustive list of online prescribing laws. SOURCE: Center for Connected Health Policy. Current State Laws and Reimbursement Policies. Fall 2019. |
|
Reimbursement and Coverage
Payment structures for telemedicine are relatively new and currently evolving; therefore, reimbursement and coverage vary by how each state chooses to regulate Medicaid and private insurance plans. Restrictions to telemedicine’s coverage often falls into one or more of the following categories:
- Provider specialty: limiting reimbursement to specific medical specialties (example: covering psychiatry and radiology but not OBGYN).
- Type of provider: limiting reimbursement to certain provider types (example: covering a visit with a physician, but not a nurse practitioner).
- Type of modality: limiting reimbursement to specific modalities (example: live video reimbursed more often than store-and-forward or remote patient monitoring).
- Patient condition: limiting reimbursement to certain conditions, like diabetes.
- Location of patient/“originating” site: limiting the location a patient can be while engaging in the telemedicine service (example: excluding the patient’s home).
Medicaid
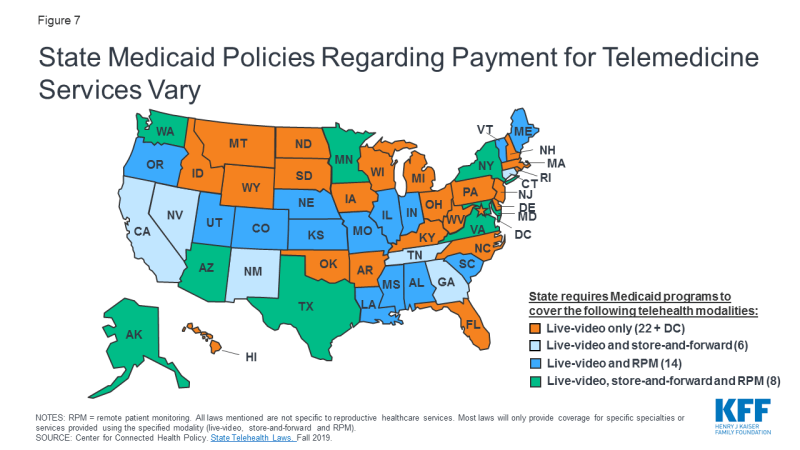
All states have laws determining which telemedicine services their Medicaid programs will cover, and for how much they will be reimbursed. These laws are not specific to reproductive health care, and may only cover certain specialties, providers, modalities, conditions and originating sites. While 50 states and D.C. reimburse for some forms of live videoconferencing, most limit coverage to certain specialties (typically behavioral health) and a few explicitly exclude OBGYN or abortion care (Appendix). Fewer states reimburse for store-and-forward services or remote patient monitoring, and often only certain services are covered like radiology or dentistry, or certain diagnoses like congestive heart failure. Eight states reimburse for some forms of all three modalities, but patients would still need to check with the specifics of their state’s plan to ensure coverage (Figure 7).
Telemedicine has the potential to increase convenience and minimize travel by allowing patients to access services from their home. However, only 19 state Medicaid programs explicitly allow the patient’s home as the originating site. In the remaining states, telemedicine may not be covered if the patient is at home or a non-clinical site. The Centers for Medicare and Medicaid Services (CMS) has shown interest in expanding the use of telemedicine; while not as applicable to most reproductive-aged individuals, CMS will expand telehealth benefits to Medicare Advantage beneficiaries in 2020, allowing a patient’s home as the originating site. State telemedicine laws are evolving, and in the future, public insurance plans may cover more services as familiarity with how to pay for this care increases.
Private insurance
KFF’s Employer Health Benefits Survey reveals coverage for telemedicine by large employers has increased significantly in recent years; the share of large firms offering telemedicine health benefits grew from 27% in 2015 to 82% in 2019, indicating promising growth for the field. 41 states and D.C. have laws governing reimbursement for telemedicine services in private plans (although laws in GA are not currently in effect). As with Medicaid, private payer laws vary based on the services, specialties and providers they cover. In approximately half of states, if telemedicine services are shown to be medically necessary and meet the same standards of care as in-person services, private insurance plans must cover telemedicine services if they would normally cover the service in-person, called “service parity.” CCHP finds only 6 states (CA, DE, GA, HI, MN, NM) require telemedicine services to be reimbursed at the same rate as equivalent in-person services, called “payment parity;” our analysis of telehealth laws suggests an additional 4 states follow payment parity as well (AR, CO, KY, NJ). In the remaining states, telemedicine is typically reimbursed at lower rates than equivalent in-person care.
Low Uptake
Based on which definition of telemedicine is used, utilization estimates vary widely. In a study by Definitive Health Care, 44% of outpatient providers reported utilizing telehealth, including applications like video conferencing, online consults, RPM and patient portals for lab results, appointment notes and prescription instructions. Uptake of telehealth appears similarly robust in a recent report, Life in Rural America; of 695 women surveyed, 26% of participants reported ever receiving a diagnosis or treatment from a provider using email, text messaging, a mobile app, live video or telephone.
By contrast, most researchers analyzing insurance claims adopt a narrower definition of telemedicine, excluding applications like phone, email and patient portals, while focusing on videoconferencing, RPM and store and forward services. Using these parameters, telemedicine utilization appears minimal. In a KFF analysis of claims data among enrollees of large employer sponsored private health plans, less than 1% of people utilized outpatient telemedicine visits in 2016. Among Kaiser Permanente patients, <5% utilized video visits from 2015-2017, but those who did reported high patient satisfaction.
Telemedicine has yet to gain traction in underserved populations; a 2013-2016 analysis published in Health Affairs revealed utilization of telemedicine among Medicaid, low income and rural populations was significantly lower than individuals with private insurance, higher incomes and in suburban and urban settings, respectively, despite most of these individuals being willing to use telemedicine. These data suggest low income and rural communities are not currently reached by telemedicine to the degree its proponents may have intended.
Investment Costs in Telemedicine Technology:
Significant logistical and financial challenges come along with establishing a telemedicine program at a health center or as a third-party app. The telemedicine platform should be compliant with the Health Insurance Portability and Accountability Act (HIPAA) and often must integrate into an existing electronic health record. This represents a significant financial investment, and outpatient centers are divided regarding their interest in telemedicine; providers cite issues such as satisfaction with their current services without telehealth, lack of clarity in reimbursement and inability to justify the investment due to lack of financial return as reasons they are not interested in investing in telemedicine services. To help with investment costs for rural providers, the Federal Communications Commission’s Rural Health Care Program has recently approved a three-year program allocating $100 million for expanding telemedicine use in low-income rural areas, offering broadband and telecommunications services at discounted prices.
Beyond startup costs, the cost of telemedicine to the health system as compared to in-person care remains unclear. Certain studies show telemedicine visits are less costly than in-person care, particularly for emergency room visits. This cost savings may be offset by increases in new utilization of the health system; one study found 88% of telehealth visits represented new utilization of the health system by those who would otherwise not seek in-person care, leading to increased overall cost. By contrast, another study found decreased follow up visits among telemedicine users, contributing to overall cost savings to the health system. As telemedicine use expands, further analysis on this topic would help elucidate the cost of telemedicine to the health system, and to patients.
Looking Forward
Access to reproductive health care, including comprehensive contraception and abortion care, is being curtailed in many communities across the U.S. While telemedicine remains a promising tool to address this unmet need, utilization of telemedicine among patients remains low. For some services, including OCP prescriptions and self-collection STI testing, telemedicine can largely function separately from the existing health system. Meanwhile for other services, including abortion care and in-lab STI testing, users must still link to in-person care, making telemedicine an adjunct to the existing health system. Notably, in-person care is still required for more effective methods of contraception like LARCs, for confirmatory testing and treatment of HIV, and for many preventative services like pap smears and pelvic exams. Significant implementation barriers exist to telemedicine’s growth, including state policies limiting its use, variable insurance coverage and high start-up investment for health centers. The future of telemedicine will likely depend on increasing availability, expanding insurance coverage and increasing reimbursement, alignment of regulatory policies and broadening outreach efforts to underserved populations who could benefit from these technologies.