The independent source for health policy research, polling, and news.
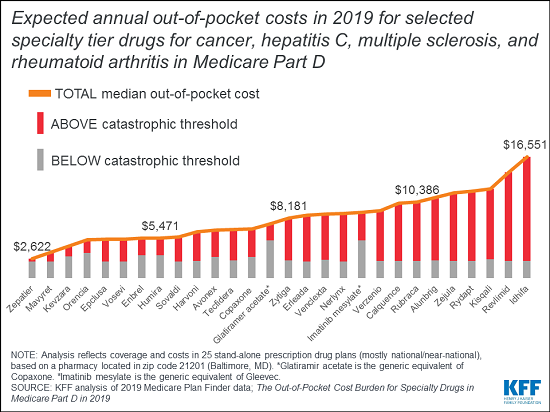
Medicare Part D Enrollees with Serious Health Conditions Can Face Thousands of Dollars in Out-of-Pocket Costs Annually for Specialty Drugs
Despite Medicare’s protections, Part D enrollees with serious health conditions can face thousands of dollars in annual out-of-pocket costs for expensive specialty drugs, a new KFF anaylsis finds.
The analysis draws on data from Medicare’s Plan Finder website to calculate expected annual 2019 costs for more than two dozen specialty tier drugs used to treat four health conditions — cancer, hepatitis C, multiple sclerosis and rheumatoid arthritis – based on coverage and costs in national and near-national stand-alone drug plans, using a pharmacy in Baltimore, MD. It found that expected median out-of-pocket costs for Part D enrollees not receiving low-income subsidies would range from $2,622 for Zepatier (for hepatitis C) to $16,551 for Idhifa (for leukemia) in 2019.
The findings come at a time when the public has expressed concern about the rising cost of prescription drugs and policymakers are considering ways to curb such spending, especially in public programs like Medicare and Medicaid.
Medicare beneficiaries continue to confront high out-of-pocket costs for specialty medications even now that the Part D coverage gap for brand-name drugs (the so-called “doughnut hole”) has been closed. Medicare requires Part D enrollees to pay 5 percent coinsurance when their total annual out-of-pocket spending exceeds an annual threshold ($5,100 in 2019), a benchmark that is commonly surpassed by beneficiaries who take just one high-priced specialty drug and people who take multiple costly drugs. The catastrophic threshold is not an absolute limit on out-of-pocket spending.
For more analysis of Medicare and prescription drug costs, including our updated 10 Essential Facts about Medicare and Prescription Drug Spending, visit kff.org.