Financial and Administrative Alignment Demonstrations for Dual Eligible Beneficiaries Compared: States with Memoranda of Understanding Approved by CMS
Using authority in the Affordable Care Act, the Centers for Medicare and Medicaid Services (CMS) has launched demonstrations that seek to improve care and control costs for people who are dually eligible for Medicare and Medicaid. Nearly 379,000 beneficiaries in nine states are enrolled in capitated models in these demonstrations as of November, 2015. Implemented beginning in July 2013, the demonstrations are changing the care delivery systems through which beneficiaries receive medical and long-term care services and the financing arrangements among CMS, the states, and providers. The demonstrations initially were approved for three years, but in July, 2015, CMS announced that states may extend their demonstrations for an additional two years. (New York’s demonstration for people with developmental disabilities (DD) is approved for four years.)
As of December, 2015, CMS has finalized memoranda of understanding (MOUs) with 13 states to implement 14 demonstrations:
- Ten states (California, Illinois, Massachusetts, Michigan, New York, Ohio, South Carolina, Rhode Island, Texas, and Virginia) are testing a capitated financial alignment model (New York is approved for two capitated demonstrations that target different populations and involve different health plans);
- Two states (Colorado and Washington) are testing a managed fee-for-service (FFS) financial alignment model; and
- One state (Minnesota) is testing the integration of administrative functions without financial alignment (Figure 1).
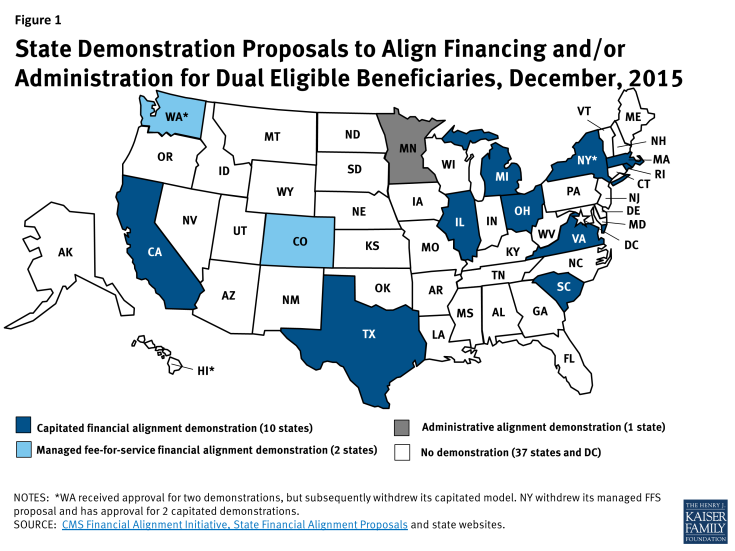
Figure 1: State Demonstration Proposals to Align Financing and/or Administration for Dual Eligible Beneficiaries, December, 2015
The status of past proposals from other states is detailed in the Appendix. This issue brief compares key provisions of the approved demonstrations, summarized in Table 1 on the next page.
| Table 1: State Dual Eligible Financial/Administrative Alignment Demonstrations Approved by CMS, December 2015 |
|||||
| State | Estimated Number of Eligible Beneficiaries | Target Population and Geographic Area | Financial Model | Earliest Effective Enrollment Date | Savings Percentage Applied to Medicare and Medicaid Contributions to Baseline Capitated Ratea |
| CA | 424,000 | Adult dual eligible beneficiaries in 7 counties | Capitated | April 2014 | 1% minimum,
1.5% maximum in year 1; 2% minimum, 3.5% maximum in year 2; 4% minimum, 5.5% maximum in year 3b |
| CO | 48,000 | Adult dual eligible beneficiaries statewide | Managed FFS | September 2014 | N/A (state shares savings with CMS retrospectively if savings and quality criteria met) |
| IL | 135,825 | Adult dual eligible beneficiaries in 21 counties grouped into 2 regions | Capitated | March 2014 | 1% in year 1;
3% in year 2; 5% in year 3 |
| MA | 90,240 | Non-elderly adult dual eligible beneficiaries in 1 partial and 8 full counties | Capitated | October 2013 | 0 in 2013;
1% in 2014 (remainder of year 1)c; 2% in year 2; >4% in year 3d |
| MI | 100,000 | Adult dual eligible beneficiaries in 25 counties grouped into 4 regions | Capitated | April 2015 | 1% in year 1;
2% in year 2; 4% in year 3, except that year 3 savings will be 3% if at least 1/3 of plans have losses exceeding 3% of revenue in year 1 |
| MN | 36,000 | Dual eligible beneficiaries age 65 and over enrolled in the Minnesota Senior Health Options program statewide | N/Ae | September 2013 | N/A (Minnesota’s demonstration will test the integration of administrative functions without financial alignment) |
| NY (LTSS) | 100,000 | Adult dual eligible beneficiaries in 8 counties who require nursing facility or nursing facility diversion and transition home and community-based waiver services or more than 120 days of community-based LTSS | Capitated | January 2015 | 1% in year 1;
1.5% in year 2; 3% in year 3, except that year 3 savings will be 2.5% if at least 1/3 of plans have losses exceeding 3% of revenue in year 1f |
| NY (DD) | 20,000 | Adult dual eligible beneficiaries in 9 counties who are eligible for state DD services and an ICF/DD level of care (must be enrolled in DD waiver if receiving waiver services) | Capitated | April 2016 | 0.25% in year 1;
0.5% in year 2; 1% in year 3, except that year 3 savings will be 0.75% if the plan has losses exceeding 3% of revenue in year 1; Year 4 savings will be the same as year 3 |
| OH | 115,000 | Adult dual eligible beneficiaries in 29 counties grouped into 7 regions | Capitated | May 2014 | 1% in year 1;
2% in year 2; 4% in year 3 |
| RI | 30,000 | Adult dual eligible beneficiaries statewide | Capitated | December 2015 | 1% in year 1;
1.25% in year 2; 3% in year 3, except that year 3 savings will be 1.5% if at least 1 plan has losses exceeding 3% of revenue in all regions in year 1 |
| SC | 53,600 | Dual eligible beneficiaries age 65 and over statewide who live in the community at the time of enrollment | Capitated | February 2015 | Same as Ohio |
| TX | 168,000 | Adult dual eligible beneficiaries with disabilities who qualify for SSI or Medicaid waiver HCBS in 6 counties | Capitated | March 2015 | 1.25% in year 1.a;g
2.75% in year 1.b;i 3.75% in year 2; 5.5% in year 3 |
| VA | 78,600 | Adult dual eligible beneficiaries in 104 localities grouped into 5 regions | Capitated | April 2014 | Same as Michiganh |
| WA | 21,000 | High cost/high risk adult dual eligible beneficiaries statewide except in 2 urban counties | Managed FFSi | July 2013 | Same as Colorado |
| NOTES: a Demonstration savings in the capitated models will be derived upfront by reducing CMS’s and the state’s respective baseline contributions to the plans by a savings percentage for each year. b California’s maximum demonstration-wide savings percentages, along with county-specific interim savings percentages, will be used to determine the demonstration’s risk corridors. c Massachusetts reduced its 2013 savings from 1% to zero. Demonstration year 1 in Massachusetts begins in 2013 and runs through December 2014. d Massachusetts anticipates savings of greater than 4% (approximately 4.2%) in year 3 to make up for forgone savings in year 1. e Minnesota’s administrative alignment demonstration will take place in its existing capitated delivery system in which Medicaid MCOs also qualify as Medicare Advantage D-SNPs. f This determination will be based on at least 15 months of data (demonstration year 1 in New York encompasses July 2014 through December 2015). g Demonstration year 1.a in Texas is March to Dec. 2015. h Demonstration year 1.b in Texas is 2016. i This determination will be based on at least 20 months of data and in all regions in which plans participate (demonstration year 1 in Virginia encompasses February 2014 through December 2015). j Washington withdrew its capitated demonstration which was approved by CMS for 2 urban counties. | |||||
Background
Dual eligible beneficiaries include seniors and non-elderly people with significant disabilities, some of whom are among the poorest and sickest beneficiaries covered by either Medicare or Medicaid. The predominant existing service delivery models for these beneficiaries typically involve little to no coordination between the two programs. Dual eligible beneficiaries account for a disproportionate share of spending in the Medicare and Medicaid programs. In the case of Medicare, this is mainly due to their relatively poorer health status, which requires higher use of medical services compared to other program beneficiaries. In the case of Medicaid, dual eligible beneficiaries’ relatively high spending is generally attributable to their greater need for LTSS.
Key Demonstration Provisions
Geographic Area and Target Population
Four states (Colorado, Minnesota, Rhode Island, and South Carolina) have statewide demonstrations, while the others are limited to certain regions.
The states’ target populations for their demonstrations vary, with ten states (California, Colorado, Illinois, Michigan, New York, Ohio, Rhode Island, Texas, Virginia, and Washington) including both elderly and non-elderly beneficiaries. Among the states targeting sub-populations:
- Massachusetts targets non-elderly people with disabilities;
- Minnesota’s administrative alignment demonstration targets elderly beneficiaries;
- South Carolina targets elderly beneficiaries who live in community-based settings at enrollment;
- One of New York’s demonstrations focuses on elderly and non-elderly beneficiaries who receive nursing facility services or nursing facility diversion and transition home and community-based waiver services or who require more than 120 days of community-based LTSS, while New York’s other demonstration focuses on beneficiaries with DD; and
- Texas targets elderly and non-elderly beneficiaries with disabilities who qualify for Supplemental Security Income (SSI) benefits or certain Medicaid home and community-based waiver services for seniors and adults with physical disabilities.
Michigan and New York are the only states with capitated demonstrations to include both beneficiaries with DD and DD services.
Enrollment
Estimated Number of Eligible Beneficiaries
CMS has stated that it plans to limit enrollment in the demonstrations to no more than two million dual eligible beneficiaries nationally. As of December, 2015, CMS has approved 14 demonstrations in which an estimated over 1.4 million beneficiaries are eligible to enroll. (Not all beneficiaries who are eligible to participate in the demonstrations are expected to enroll.) The estimated number of beneficiaries eligible for California’s demonstration is just under 30 percent of the total number of beneficiaries eligible for all demonstrations approved to date and exceeds the number of eligible beneficiaries in each of the other states with approved demonstrations. Enrollment in Los Angeles County, capped at 200,000 beneficiaries, will be greater than the number of beneficiaries eligible to participate in any other state’s demonstration (Figure 2).
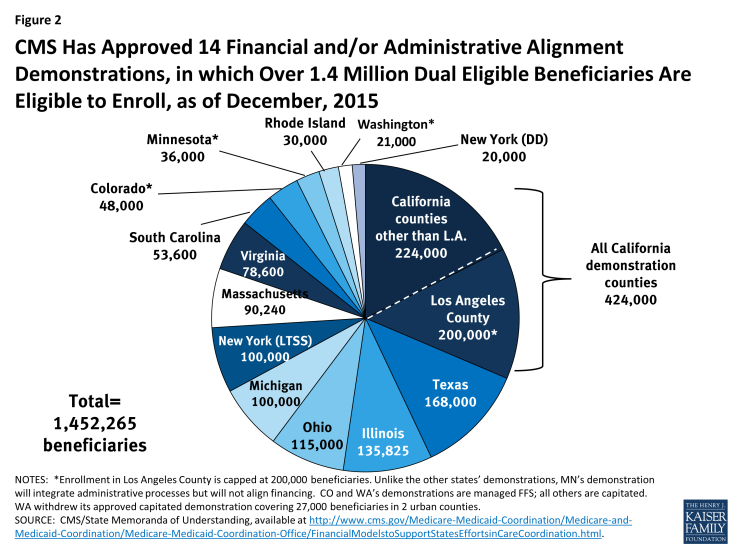
Figure 2: CMS Has Approved 14 Financial and/or Administrative Alignment Demonstrations, in which Over 1.4 Million Dual Eligible Beneficiaries Are Eligible to Enroll, as of December, 2015
Enrollment Timeline
Enrollment has begun in all of the states with demonstrations approved to date except Rhode Island, which will begin its demonstration no sooner than December, 2015, and New York’s demonstration for beneficiaries with DD, which will begin no sooner than April, 2016. States vary in the amount of time that beneficiaries have been enrolled in their demonstrations: some states have enrolled beneficiaries for more than two years (Washington, Massachusetts), while other states began enrolling beneficiaries in early 2015 (New York, South Carolina, Texas, Michigan) (Figure 3).
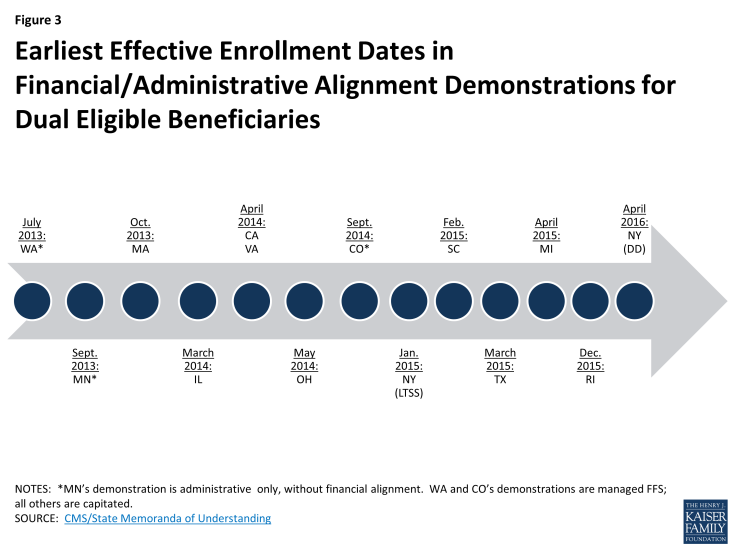
Figure 3: Earliest Effective Enrollment Dates in Financial/Administrative Alignment Demonstrations for Dual Eligible Beneficiaries
Enrollment Process and Beneficiary Choices
Nearly all of the capitated demonstrations (except for some counties in California, in which beneficiaries are automatically enrolled in the demonstration without an initial voluntary enrollment period) began with a voluntary enrollment period in which beneficiaries could “opt in” to the demonstration and select a managed care plan (Rhode Island also plans to begin with a voluntary opt in period). The voluntary enrollment period in nearly all states is followed by passive enrollment periods in which the remaining beneficiaries will be automatically assigned to a managed care plan; however, enrollment in New York’s demonstration for beneficiaries with DD will remain voluntary only. To effectuate passive enrollment, states are developing “intelligent assignment” algorithms to preserve continuity of providers and services when assigning beneficiaries to plans.
Beneficiaries retain the right to opt out of the demonstration at any time but must take affirmative action to do so. In all states, beneficiaries can opt out of the demonstration and choose another delivery system (i.e., FFS, Medicare Advantage, Program of All-Inclusive Care for the Elderly) for their Medicare benefits. However, states may seek CMS approval to require beneficiaries to enroll in Medicaid managed care even if they opt out of the financial alignment demonstration for their Medicare benefits, and five states with capitated demonstrations (California, Illinois, New York’s LTSS demonstration, Ohio, and Texas) have indicated that they are doing so. By contrast, six states with capitated demonstrations (Massachusetts, Michigan, New York’s DD demonstration, Rhode Island, South Carolina, and Virginia) allow beneficiaries who opt out of the demonstration to remain in the FFS delivery system for both their Medicare and Medicaid benefits (Table 2).
| Table 2: Beneficiary Enrollment Choices in the Capitated Financial Alignment Demonstrations |
||
| State | Managed Care Enrollment Required for: | |
| Medicare | Medicaida | |
| California | No | Yesb |
| Illinois | No | Yesc |
| Massachusetts | No | No |
| Michigan | No | No |
| New York – LTSS | No | Yesd |
| New York – DD | No | No |
| Ohio | No | Yese |
| Rhode Island | No | No |
| South Carolina | No | No |
| Texas | No | Yesf |
| Virginia | No | No |
| NOTES: a CMS approval is necessary for states to require beneficiaries to enroll in Medicaid managed care, even if beneficiaries opt out of the financial alignment demonstration for their Medicare benefits. b California’s § 1115 waiver was amended to require beneficiaries to enroll in managed care plans for their Medicaid benefits, including LTSS. c Illinois has a draft § 1115 waiver application seeking to require Medicaid managed care enrollment. d New York’s § 1115 waiver requires beneficiaries in the financial alignment demonstration geographic area who receive more than 120 days of LTSS to enroll in a Medicaid MLTSS plan. e Ohio’s MOU indicates that the state may seek additional § 1915(b)/(c) waiver authority to require beneficiaries to enroll in Medicaid managed care. f Texas’s existing § 1115 waiver requires adult dual eligible beneficiaries to enroll in Medicaid managed LTSS.
SOURCE: KCMU analysis of states’ financial alignment demonstration memoranda of understanding with CMS, available at http://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/FinancialModelstoSupportStatesEffortsinCareCoordination.html. |
||
Given the complexities of the enrollment decision, beneficiaries are likely to need individual in-person options counseling to make their choice. Seven states (California, Illinois, Massachusetts, Michigan, New York, Virginia, and Washington) have received CMS funding to date to support beneficiary outreach, education, and options counseling in their demonstrations through their State Health Insurance Program and Aging and Disability Resource Centers.
In Washington’s managed FFS demonstration, beneficiaries are automatically enrolled in a health home network but retain the choice about whether to receive Medicaid health home services; other Medicare and Medicaid services will continue to be provided on a FFS basis. Similarly, in Colorado’s managed FFS demonstration, beneficiaries will be automatically assigned to the Regional Care Collaborative Organization in their geographic area to access care coordination services but may disenroll from the demonstration at any time.
Minnesota’s administrative alignment demonstration does not involve passive enrollment; instead enrollment in Senior Health Options plans remains voluntary, although the demonstration will test an integrated enrollment system.
Care Delivery Model
The ten states with capitated demonstrations are using managed care plans to coordinate services for beneficiaries through a person-centered planning process. Person-centered planning focuses on the strengths, needs, and preferences of the individual beneficiary instead of being driven by the care delivery system.
Some states require or allow their managed care plans to contract with other entities to provide services in their demonstrations (Table 3). Massachusetts requires its plans to contract with community-based organizations to provide Long-Term Supports coordinators as independent members of the beneficiary’s care team, Michigan requires its plans to contact with existing Medicaid Prepaid Inpatient Health Plans (PIHPs) to provide behavioral health services, and Ohio requires its plans to contract with Area Agencies on Aging to coordinate home and community-based waiver services for enrollees over age 60. (Illinois, New York, Rhode Island, South Carolina, Texas, and Virginia’s MOUs do not include any similar requirements). California requires its plans to establish MOUs with county behavioral health agencies to provide specialty mental health services and with county social services agencies to coordinate In Home Supportive Services. Demonstration health plans in Los Angeles County are subcontracting with other Medicare Advantage plans to offer a variety of benefit packages to enrollees in California’s demonstration.
Washington’s managed FFS demonstration is using Medicaid health home care coordination organizations to manage services among existing Medicare and Medicaid providers, and Colorado is using its existing Medicaid Accountable Care Collaborative program to coordinate Medicare and Medicaid services for beneficiaries in its demonstration.
Minnesota’s administrative alignment demonstration maintains the existing Senior Health Options program delivery system in which Medicaid managed care plans contract with the state and also are qualified as Medicare Advantage Special Needs Plans focused on dual eligible beneficiaries (D-SNPs) under contract with CMS.
Financing
Ten states (California, Illinois, Massachusetts, Michigan, New York, Ohio, Rhode Island, South Carolina, Texas, and Virginia) are testing CMS’s capitated financial alignment model, in which managed care plans will receive capitated payments from CMS for Medicare services and the state for Medicaid services.
Anticipated program savings in the capitated financial alignment demonstrations are deducted up-front from CMS’s and the state’s respective baseline contributions to health plans by a savings percentage for each year (Table 1). CMS will contribute the Medicare portion of the capitated rate and recently announced rate adjustments for 2016, to better align capitated payments with fee-for-service costs for full benefit dual eligible beneficiaries. The Medicaid portion of the capitated rate includes both the federal and state funding. None of the MOUs explicitly states the basis for the savings percentages, although Illinois’ MOU notes that it currently has one of the highest rates of potentially avoidable hospital admissions among dual eligible beneficiaries nationally and one of the highest proportions of spending on institutional services compared to HCBS. While California’s MOU specifies minimum savings percentages of 1% in year one, 2% in year two, and 4% in year three, it also includes maximum savings percentages of 1.5% in year one, 3.5% in year two, and 5.5% in year three, making the maximum savings percentages in California among the highest of the approved demonstrations to date. Texas’s MOU specifies savings percentages of 1.25% in year 1.a (March to December 2015), 2.75% in year 1.b (2016), 3.75% in year 2, and 5.5% in year 3.
All 10 states with capitated financial alignment demonstrations include provisions to withhold a portion of the capitated rate that plans can earn back if specified quality measures are met. California also requires its plans to provide incentive payments from the quality withhold funds to county behavioral health agencies based on achievement of service coordination measures, and Michigan requires its plans to reward the PIHPs that will provide behavioral health services when the plan earns the withheld payment. South Carolina plans must provide financial incentives to providers that achieve NCQA patient-centered medical home certification.
Two states (Colorado and Washington) are testing CMS’s managed FFS model in which providers will continue to receive FFS reimbursement for both Medicare and Medicaid-covered services. Any savings in these demonstrations will be determined retrospectively, with the state eligible to share in savings with CMS if savings targets and quality standards are met.
Minnesota’s administrative alignment demonstration will not test one of CMS’s financial alignment models. Instead, Minnesota’s Senior Health Options program will maintain its existing capitated integrated payment and delivery system arrangements involving Medicaid MCOs that also qualify as Medicare Advantage D-SNPs. Plans will be allowed to integrate Medicare and Medicaid primary care payments to promote care coordination through health care homes and improved coordination among primary, acute, and LTSS and among physical and behavioral health services.
Benefits
The 10 states with capitated financial alignment demonstrations include nearly all Medicare and Medicaid services in the plans’ benefits package and capitated payment. All states include nursing facility services in the plans’ capitated payment and benefits package. Eight of the 10 states testing the capitated model (Illinois, Michigan, New York (both demonstrations), Ohio, South Carolina, Rhode Island, Texas, and Virginia) include beneficiaries who receive certain Medicaid home and community-based waiver services, while two states (California and Massachusetts) exclude all HCBS waiver enrollees from their demonstrations. Plans are allowed to offer additional benefits, outside the traditional Medicare and Medicaid benefits packages, as appropriate to beneficiary needs. All states require their health plans to offer beneficiaries the option to self-direct their LTSS (Table 3).
Five of the capitated states require plans to offer additional benefits as part of the demonstration. Massachusetts plans must offer certain diversionary behavioral health and community support services that are not otherwise covered as well as expanded Medicaid state plan benefits. Ohio’s § 1915(b)/(c) Medicaid waiver, which operates concurrently with the demonstration, includes expanded Medicaid state plan benefits and additional HCBS. California’s demonstration includes vision and non-emergency medical transportation benefits, and its plans may offer additional HCBS. South Carolina’s demonstration includes a palliative care benefit for enrollees with a serious, chronic or life-threatening illness who may not meet hospice criteria. Michigan’s health plans must offer adaptive medical equipment and supplies, community transition services, fiscal intermediary services to support self-direction, personal emergency response systems, and respite services (Table 3).
| Table 3: LTSS in the Capitated Financial Alignment Demonstrations |
|||||||
| State | Nursing facility services included | Home and community-based waiver services included | DD population/ services included | Traditional Medicaid benefits package expanded | Plans can offer supplemental benefits | Self-direction option required | Required contracting/service coordination |
| CA | Yes | No | No | Yes – plans must provide vision and non-emergency medical transportation services | Yes | Yes | Yes – plans must have MOUs with county mental health and substance use agency for behavioral health services and county social service agency for IHSS |
| IL | Yes | Yes (except DD) | No | Not mentioned in MOU | Yes | Yes | Not mentioned in MOU |
| MA | Yes | No (may seek to include in future) | No | Yes – plans must provide diversionary behavioral health and community support services and (unspecified) expanded Medicaid state plan benefits | Yes | Yes | Yes – plans must provide Long-Term Supports coordinator form independent community-based organization as a member of the care team |
| MI | Yes | Yes | Yes | Yes – plans must provide adaptive medical equipment and supplies, community transition services, fiscal intermediary for self-direction, personal emergency response system, respite | Yes | Yes | Yes – plans must contract with PIHP for behavioral health services |
| NY – LTSS | Yes | Yes (NF diversion and transition waiver only) | No* | Not mentioned in MOU | Yes | Yes | Not mentioned in MOU |
| NY – DD | Yes (ICF/DD also included) | Yes (DD only) | Yes | No | Yes | Yes | Not mentioned in MOU |
| OH | Yes | Yes (except DD) | No | Yes – expects to require plans to provide (unspecified) expanded Medicaid state plan benefits and additional HCBS | Yes | Yes | Yes – plans must contract with AAA to coordinate HCBS for beneficiaries over age 60 |
| RI | Yes | Yes (except DD) | DD population enrolled but LTSS excluded | Not mentioned in MOU | Yes | Yes | Not mentioned in MOU |
| SC | Yes | Yes (elderly/disabled, HIV/AIDS, and mechanical ventilation waivers only) | No | Yes – plans must provide palliative care benefit | Yes | Yes | Not mentioned in MOU |
| TX | Yes | Yes (seniors and people with physical disabilities who meet NF level of care only) | No | Not mentioned in MOU | Yes | Yes | Not mentioned in MOU |
| VA | Yes | Yes (elderly/disabled with consumer direction waiver only) | No | Not mentioned in MOU | Yes | Yes | Not mentioned in MOU |
| WA | Yes | Yes (except DD) | No | Not mentioned in MOU | Yes | Yes | Not mentioned in MOU |
| SOURCE: KCMU analysis of states’ financial alignment demonstration memoranda of understanding with CMS, available at http://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/FinancialModelstoSupportStatesEffortsinCareCoordination.html. | |||||||
Washington’s managed FFS demonstration adds Medicaid health home services but does not otherwise change the existing Medicare and Medicaid benefits packages. Similarly, Colorado offers care coordination services but otherwise does not change the existing Medicare and Medicaid benefits packages.
Minnesota’s administrative alignment demonstration will continue to provide Medicare benefits at least equivalent to the basic benefit levels included in Medicare Parts A, B, and D and Medicaid benefits based on existing Medicaid MCO contracts.
Demonstration Ombudsman
CMS has announced a funding opportunity for states with approved MOUs to support the planning, development, and provision of independent ombudsman services in the demonstrations, with ten states (California, Colorado, Illinois, Massachusetts, Michigan, Ohio, Rhode Island, South Carolina, Virginia, and Washington) awarded funding to date. Seven states (Colorado, Illinois, Michigan, Ohio, South Carolina, Texas, and Washington) are using an ombuds office within state government, although independent of the state Medicaid agency, while four states (California, Massachusetts, New York, and Virginia) are using an ombuds entity outside of state government. Minnesota’s MOU provides that the state’s managed care ombudsman will provide input on plan and system-wide performance but does not provide further details.
Appeals
All of the capitated demonstrations provide beneficiaries with a single integrated notice of appeal rights, and the existing Medicare Part D appeals process for prescription drugs will continue to apply in all demonstrations. Minnesota’s administrative alignment demonstration is building on the integrated appeals system already established in its Senior Health Options program by adding a single integrated notice of appeal rights and standardizing the timeframes to request Medicare and Medicaid appeals. By contrast, Colorado and Washington’s managed FFS demonstrations do not make any changes to the existing Medicare and Medicaid appeals systems.
New York’s two capitated financial alignment demonstrations include a fully integrated four level appeals process for all services traditionally covered by Medicare Parts A and B and Medicaid. New York requires its demonstration health plans to continue providing benefits while appeals are pending for both prior-approved Medicare and Medicaid services if the beneficiary so requests within 10 days of the date of the notice. (Continued benefits pending appeal is currently available under federal law for Medicaid services but not for Medicare services.)
Five of the capitated demonstration states (Illinois, Massachusetts, Rhode Island, South Carolina, and Virginia) require beneficiaries to first exhaust an internal health plan appeal before proceeding to external appeals, while four of the capitated demonstration states (California, Michigan, Ohio, and Texas) allow beneficiaries to choose whether to first file an internal health plan appeal or instead to proceed directly to a fair hearing for Medicaid-covered services.
All of the capitated demonstrations require health plans to continue Medicare and Medicaid benefits while internal health plan appeals are pending; beneficiaries may request that Medicaid benefits continue while fair hearings are pending, but Medicare benefits will not continue during external appeals. (California’s aid pending appeal provision is contained in its three-way contract instead of its MOU.) California’s MOU provides that the existing Medicare and Medicaid appeals processes will continue at least through demonstration year one, and the state will work to create a more integrated appeals process in future years.
Looking Ahead
As the demonstrations are implemented, additional details about several features are emerging, including how beneficiaries are being notified, counseled, and enrolled; how the demonstrations are being monitored and overseen; how beneficiary ombuds programs are being implemented; and how the demonstrations are being evaluated. CMS has contracted with RTI International to conduct an overall evaluation of the demonstrations as well as state-specific evaluations. The MOUs provide that the evaluations will include site visits, analysis of program data, focus groups, key informant interviews, analysis of changes in quality, utilization, and cost measures, and calculation of savings attributable to the demonstrations. The evaluation findings are to be reported quarterly, although there is likely to be a lag in data availability.
The approved MOUs provide additional information about how CMS and the states envision the demonstrations working and insight into the framework and policy decisions that CMS may apply when developing MOUs with other states that submitted proposals. Additional details are specified in the three-way contracts between CMS, the state, and demonstration plans in the capitated model, in the states’ final demonstration agreement with CMS in the managed FFS model, and in policy guidance. Key areas to continue to consider as the demonstrations are implemented include:
- how beneficiaries are making their enrollment choices;
- what the actual sources of program savings will be;
- how beneficiaries’ access to medically necessary services and supports is being ensured;
- how the demonstrations are affecting beneficiary access to HCBS;
- how beneficiaries are navigating the demonstrations’ grievance and appeals processes;
- whether continuity of care and intelligent assignment provisions are sufficient to prevent care disruptions and the extent to which beneficiaries’ current providers are participating in demonstration health plan networks;
- how plans and providers are accommodating the needs of beneficiaries with disabilities; and
- what impact the demonstrations are having on care quality and health outcomes.
While the demonstrations offer the potential opportunity to improve care coordination, lower program costs, and achieve outcomes such as better health and the increased use of HCBS instead of institutional care, at the same time the high care needs of many dual eligible beneficiaries increases their vulnerability when care delivery systems are changed.


