Federal Medicaid Outlays During the COVID-19 Pandemic
This data note analyzes federal Medicaid outlays before and during the COVID-19 pandemic. In the one year since the onset of the pandemic, federal Medicaid outlays totaled $500.8 billion and grew by 19.5%, compared to 6.3% growth in the one year before the pandemic. The first fiscal quarter of the pandemic (April to June 2020) saw particularly high outlays due to the beginning of enhanced federal Medicaid funds. Outlays remained high in the following three quarters (July 2020 through March 2021), reflecting this continued enhanced federal match as well as increased enrollment.
The outlay data analyzed in this data note comes from The Monthly Treasury Statement of Receipts and Outlays of the United States Government. The Bureau of the Fiscal Service (part of the U.S. Department of the Treasury) publishes these Monthly Treasury Statements, which summarize the financial activities of the U.S. federal government including receipts and outlays of funds. Specifically, this data note analyzes the Treasury data on outlays of the federal government classified as “grants to states for Medicaid.”1 This analysis examines quarterly and yearly outlays to understand the implications of the pandemic and the enhanced federal matching funds. Prior to the pandemic, states reported only incremental changes to Medicaid enrollment and spending, generally driven by rising prescription drug costs, incremental provider rate increases, and, in a small number of states, recent implementation of the Affordable Care Act (ACA) Medicaid expansion.2 Comparing quarterly outlays for the years before and during the pandemic allows for a comparison to what may be more typical quarterly variation.
As part of the federal response to the COVID-19 pandemic, states may access enhanced federal Medicaid funds. States and the federal government jointly finance Medicaid. The pandemic has generated both a public health crisis and an economic crisis, with major implications for Medicaid, a countercyclical program. During economic downturns, more people enroll in Medicaid as incomes fall, increasing program spending at the same time state tax revenues may be falling. To both support Medicaid and provide broad fiscal relief as state revenues declined precipitously, the Families First Coronavirus Response Act (FFCRA) authorized a 6.2 percentage point increase in the federal Medicaid match rate (“FMAP”) (retroactive to January 1, 2020) available if states meet certain “maintenance of eligibility” (MOE) requirements. This FMAP increase does not apply to the Affordable Care Act expansion group, for which the federal government already pays 90% of costs. States could draw down the increased federal matching funds beginning at the end of March for claims paid in the first quarter of 2020 and in early April for the second quarter of 2020.3 The FMAP increase will expire at the end of the quarter in which the public health emergency (PHE).
In the one year since the onset of the coronavirus pandemic, federal Medicaid outlays grew by 19.5%, compared to 6.3% growth in the one year before the pandemic (Figure 1). Total outlays in the four fiscal quarters since the pandemic (April 2020 through March 2021) were $500.8 billion, representing a 19.5% increase over the prior year’s outlays of $419.1 billion. After the onset of the COVID-10 pandemic and the passage of the FFCRA in March 2020, quarterly outlays in Quarter 3 of FFY 2020 (April through June 2020) were $127.4 billion, an increase of 22.5% over Quarter 3 outlays in the prior year. This initial increase likely reflects Medicaid claims retroactive to January that were made available at the end of March as well as enhanced matching funds for the second quarter. After this initial spike in outlays immediately following the FMAP increase, quarterly outlays have been somewhat lower but still significantly higher than the prior year. This trend reflects the continued enhanced federal match as well as increased enrollment due to requirements that states maintain continuous coverage for Medicaid enrollees to access the enhanced match and also to the economic downturn.
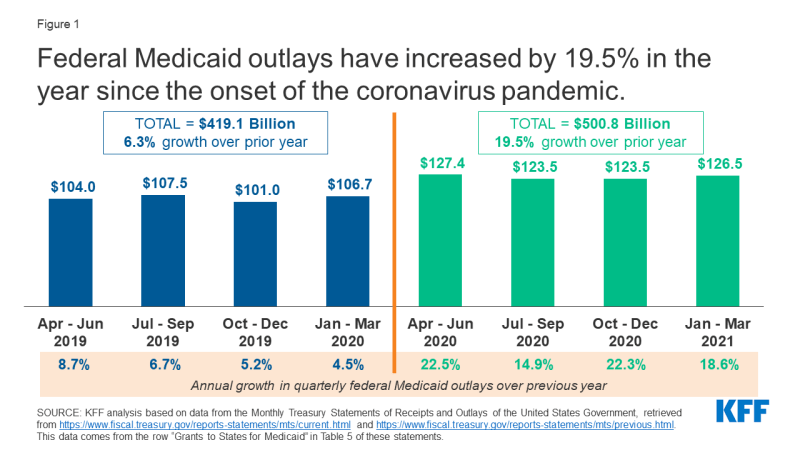
Figure 1: Federal Medicaid outlays have increased by 19.5% in the year since the onset of the coronavirus pandemic.
Continued growth in federal Medicaid outlays through March 2021 (the end of the second quarter of FFY 2021) likely reflects federal matching for increased state Medicaid spending during the pandemic. National data shows an increase in Medicaid enrollment of 10.8% from February to November 2020, a reversal of trends prior to the pandemic when enrollment was declining. While the enhanced FMAP shifts some state spending on this increased enrollment to the federal government, the sustained federal outlay growth in the quarters after the FMAP increase first took effect likely reflects overall Medicaid spending growth that is experienced at the state-level as well as the federal level. State spending growth during the pandemic likely varies across states based on economic conditions as well as the populations experiencing increased enrollment in each state (for example, increases in expansion enrollment would result in smaller increases in state spending due to the 90% federal match rate for this population).
The duration of federal fiscal relief to state Medicaid programs during the pandemic, which will affect both state and federal Medicaid spending in the future. The enhanced FMAP provides federal fiscal relief that helps replace state spending, so federal Medicaid spending growth may continue to outpace state spending growth while the enhanced FMAP is in place. When the fiscal relief expires, federal spending growth will fall and state spending growth will increase sharply. Although the current PHE declaration expires on July 20, 2021 (which means the enhanced FMAP is slated to expire at the end of September 2021), the Biden Administration has indicated that the PHE will likely remain in place throughout 2021 and that states will receive 60 days’ notice prior to its expiration or termination. This announcement means that the FMAP increase is likely to continue through at least the end of March 2022. The American Rescue Plan Act of 2021 expanded the FMAP to 100% for the administration of COVID-19 vaccines to Medicaid enrollees and also provided options for states to receive additional temporary FMAP increases, including for expanded home and community-based services and as an incentive for new adoption of the ACA Medicaid expansion. These increases will likely shift additional Medicaid spending from states to the federal government.
Endnotes
The March 2021 Monthly Treasury Statement can be accessed at https://www.fiscal.treasury.gov/reports-statements/mts/current.html and all others included in this data note (April 2018 through February 2020) can be accessed at https://www.fiscal.treasury.gov/reports-statements/mts/previous.html. The data included in this date note is from the row titled “Grants to States for Medicaid” in Table 5 of these statements, titled “Outlays of the U.S. Government.” These grants to state Medicaid programs are included in the federal government’s total outlays to the Department of Health and Human Services. These grants do not include outlays to the Children’s Health Insurance Fund (CHIP).
Two states (Maine and Virginia) implemented Medicaid expansion under the ACA in January 2019 and two others states (Idaho and Utah) implemented the expansion in January 2020. These expansions may contribute to higher federal Medicaid outlays in the quarter that expansion was implemented. Similarly, Nebraska’s implementation of expansion in October 2020 may contribute to higher federal Medicaid outlays in the first quarter of FFY 2021.
CMS, COVID-19 FAQs for State Medicaid and CHIP Agencies, Section 5.F (updated as of 1/6/2021), https://www.medicaid.gov/state-resource-center/downloads/covid-19-faqs.pdf.
