Impact of Coronavirus on Community Health Centers
Background
Community health centers are a national network of safety net primary care providers that fill an important role in national, state, and local responses to the coronavirus pandemic. Health centers primarily contribute to response efforts by providing tests, triaging patients, and reducing the burden on hospitals, although they also play a role in addressing demand for behavioral health services and continuing primary care for patients with chronic conditions. Patients at health centers are disproportionately low-income and people of color, groups especially hard hit by the pandemic. Among the roughly 28 million patients served by health centers, 91% are low-income and 63% are racial or ethnic minorities. Like other outpatient health care providers, health centers are having to adjust to stay-at-home orders, drops in patient visits for non-essential health care, and workforce challenges. This brief presents findings from new data collected by the Health Resources and Services Administration (HRSA) to provide insights into how health centers are adapting their services in response to the pandemic and how coronavirus is affecting their operations and long-term financial outlook with patient visits and revenue from those visits dropping precipitously. (For more detail on the data underlying this Data Note, see the text box at the end of the brief.)
COVID-19 Testing at Health Centers
Nine out of ten (90%) health centers are providing COVID-19 tests, and in 16 states and DC, all health centers are providing tests. Of those that provide testing, the majority (67%) offer walk-up or drive-through testing as of May 8, which can expand access to testing. In the week preceding May 8, health centers reported providing 127,816 tests, with 36,155 patients (28%) testing positive, roughly double the national positive test rate of 13% during a similar period.
People of color represented more than half of all people tested (57%) and confirmed cases (56%) at health centers. Among all individuals receiving tests, 24% were White and 57% were among people of color, including 32% who were Hispanic and 16% who were Black (Table 1). Race/ethnicity was unknown for about 1 in 5 tests (19%) and 1 in 4 confirmed cases (24%). Hispanics made up a higher share of positive tests, compared to their share of total tested patients (42% vs. 32%), while White patients made up a slightly lower share of positive tests compared to their share of total tested patients (19% vs. 24%). The ability of health centers to report testing data by race/ethnicity is important for broader efforts to ensure access to COVID-19 testing for people of color and to address disparities that existed prior to COVID-19 and may be widening due to the pandemic.
| Table 1: Share of COVID-19 Tests and Confirmed Cases at Health Centers by Race and Ethnicity, Week Ending May 8, 2020 | ||
| Race/Ethnicity | Percent of Tests | Percent of Positive Tests |
| White | 23.7% | 19.5% |
| Hispanic | 32.2% | 42.5% |
| Black | 15.8% | 7.0% |
| Asian | 1.9% | 1.1% |
| American Indian/Alaska Native | 1.1% | 0.3% |
| Native Hawaiian/Other Pacific Islander | 0.4% | 0.4% |
| More than One Race | 5.9% | 4.8% |
| Unknown Race/Ethnicity | 19.0% | 24.4% |
| Total | 100% | 100% |
| NOTES: Persons of Hispanic origin may be of any race. For this analysis, Hispanic patients include those who report Hispanic ethnicity and White, Black, or unknown race. Patients classified as White or Black are non-Hispanic. Other racial categories include both Hispanic and non-Hispanic individuals. SOURCES: HRSA. Health Center COVID-19 Survey. Latest data for the week ending May 8, 2020. |
||
Effects of Coronavirus on Health Center Operations
Despite ramping up testing and virtual visits, health centers are reporting steep declines in patient visits and many staff who are unable to work. Health center organizations reported a 43% drop in the number of patient visits compared to before the pandemic, as many people across the country are avoiding non-essential trips to health care providers. The drop in visits comes even after health centers have been increasing the number of telehealth visits, with health centers conducting roughly half (51%) of visits virtually or over the phone. Additionally, health centers report that 11% of staff are not working due to exposure to the coronavirus, lack of protective equipment, site closures, or family obligations, among other reasons.
There have been 1,954 temporary health center site closures due to repercussions from the coronavirus as of May 8. Most health centers operate multiple service delivery sites – in 2018, 1,362 health centers operated 11,744 sites. The number of temporary site closures likely undercounts total closures, given that more than a quarter of health centers did not respond to the survey and are not included in the total. The survey data also do not provide details on the types of sites that have closed, such as whether the closed sites are brick-and-mortar, mobile vans, or school-based clinics. Still, site closures are occurring in states hard hit by the virus as well as in states less affected. Connecticut, close to the epicenter of the pandemic in the US, has seen nearly three-quarters (73%) of its sites closed, while Kentucky and Mississippi, which had fewer cases, have each seen 49% of sites closed. At least one-third of sites have closed in Nebraska (48%), Kansas (36%), West Virginia (36%), and Michigan (33%).
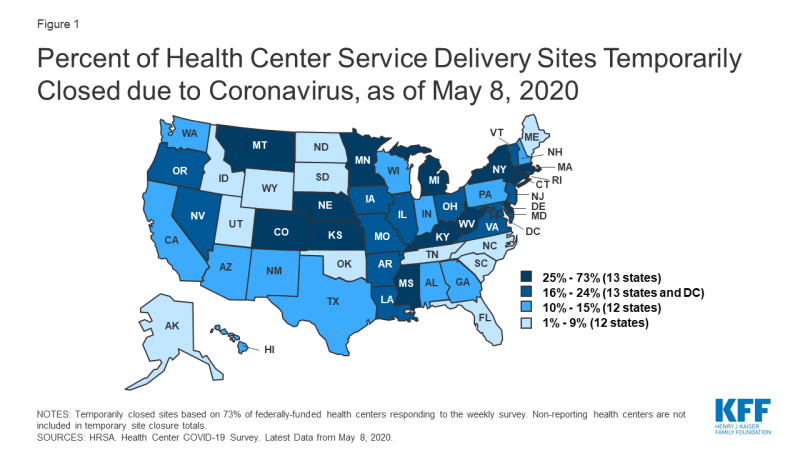
Figure 1: Percent of Health Center Service Delivery Sites Temporarily Closed due to Coronavirus, as of May 8, 2020
Financial Challenges
Health centers have received $1.98 billion in rapid response grants from the federal government, though more financial support may be needed to sustain services. These grants include $100 million in emergency grant funding and $1.3 billion through the Coronavirus Aid, Relief and Economic Security Act (CARES) that can be used to support response efforts, including buying testing materials and personal protective equipment (PPE), as well as to maintain or increase health center capacity generally. In early May, health centers received $583 million in grants to support COVID-19 testing capacity through the Paycheck Protection Program and Health Care Enhancement Act. All federally-funded health centers received each of these grants through an expedited awards process based on the size of the health center patient population and the number of uninsured patients reported to the Uniform Data System. While this funding is significant in aiding the coronavirus response, the combined $1.98 billion in additional appropriations represents just 7% of total health center revenues in 2018 (the most recent year of data available). Although data on the impact of the pandemic on overall health center finances are not available, the majority of health center revenues (68%) come from patient visits, and the drop in those visits could be contributing to a roughly 30% decrease in health center revenues. Adding to the uncertainty for health centers’ finances is the Community Health Center Fund (CHCF), an important source of federal funding representing $4 billion of the $5.6 billion appropriated to health centers in FY 2019. The CHCF has been extended through November – though it has not been reauthorized longer term as of mid-May 2020.
The effects of patient declines and staffing issues could have major implications for health centers even after the pandemic. Leading up to the pandemic, the two most commonly cited challenges for health centers were financial and workforce issues, both of which have been exacerbated by the economic effects of the coronavirus. The precipitous drop in patient volume has likely led to steep declines in patient care revenue that may contribute to future financial instability. Depending on how long the crisis lasts, some of the temporary site closures and staff reductions could become permanent, further exacerbating long-standing health care access issues in communities served by health centers.
Conclusion
Health centers will continue to play an important role in responding to the coronavirus pandemic and in providing access to care for communities disproportionately affected by COVID-19, especially as job losses mount and the number of people who are uninsured or covered by Medicaid rises. However, key findings from the HRSA survey highlight the significant operational challenges health centers are facing, which threaten their longer-term financial viability. While the emergency federal funding provided so far has aided health centers’ coronavirus response, secure future funding will also be important to maintain the long-term viability of the primary care safety net after the pandemic is over.
About the Health Center COVID-19 Data
In April 2020, HRSA began a weekly, rapid-response survey of all federally-funded health centers to track the impact of the coronavirus on health centers and identify needs for training, technical assistance, funding, and other resources. The survey instrument asks health centers to report on experiences from the previous week. All findings are reported at the health center organization level, although most health center organizations operate multiple clinic sites. Unless otherwise specified, all results discussed in this Data Note report findings at the health center organization (versus site) level. HRSA reports findings from the data as unweighted totals and percentages that do not account for non-responding health centers. The most recent survey data in this report is based on responses from the week ending May 8, 2020, with 1,011 (73%) federally-funded health centers responding to the survey.
