Advancing Opportunities, Assessing Challenges: Key Themes from a Roundtable Discussion of Health Care and Health Equity in the South
Introduction
In late March 2014, the Kaiser Family Foundation’s Commission on Medicaid and the Uninsured and the Satcher Health Leadership Institute gathered a broad range of stakeholders at Morehouse School of Medicine in Atlanta, Georgia for a roundtable discussion of current and future opportunities and challenges for advancing health care and health equity in the South. Roundtable participants represented nearly every state within the South and a broad range of perspectives, including health policy researchers, providers and hospitals, state officials, and consumer advocates. This brief summarizes the primary themes expressed by participants as well as next steps to consider. Many of the themes that arose as part of this discussion apply to the nation more broadly but have particular resonance and importance for the South given the region’s longstanding disparities in health and health care. Companion materials, including Health Coverage and Care in the South in 2014 and Beyond and Health Coverage and Care in the South: A Chartbook, provide information on health coverage and care today in the South and changes under the Affordable Care Act (ACA).
Background
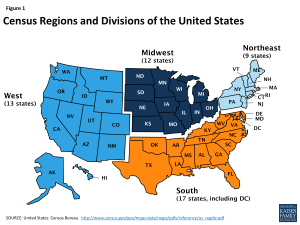
The American South comprises a significant share of the nation’s population and some of the nation’s poorest states. As defined by the U.S. Census Bureau, the American South encompasses 17 states (Figure 1). The region is home to 115 million individuals, who account for over a third (37%) of all U.S. residents, and is growing rapidly. The South is racially and ethnically diverse, with people of color making up 41% of the total southern population. Although the region’s poverty rate is not significantly different from the national rate, with about one in five non-elderly Southerners living in a poor household, the South includes states with some of the highest poverty rates in the nation, such as Louisiana (28%), Mississippi (28%), Arkansas (26%), and the District of Columbia (25%).
The South is undergoing demographic shifts that will shape health care and health equity moving forward. Specifically, the population is growing rapidly within urban areas, while rural areas are experiencing declining or slow population growth. In addition, the region is becoming increasingly diverse, with a steadily increasing Black population and a rapidly growing Hispanic population. These changes are occurring together with growing educational disparities compared to the rest of the country and an increasingly aging population.
Southerners face longstanding disparities in health and health care. While measures of health status vary by state, Southerners as a group generally are more likely than those in other regions to have a number of chronic illnesses and experience worse health outcomes. As in other regions, health status within the South also varies by race and ethnicity and Blacks, in particular, are more likely than Whites to report fair or poor health. While a broad array of factors contributes to these disparities in health, they, in part, reflect the fact that Southerners are more likely to be uninsured and less likely to have access to needed health care services than those in other regions.
The ACA offers new opportunities to advance health and health equity in the South. The ACA provides new coverage options for millions of uninsured Southerners, particularly in states that are implementing the ACA Medicaid expansion. Moreover, the ACA includes a wide array of provisions designed to improve health care delivery systems, increase access to care, enhance prevention and wellness efforts, and reduce disparities, which together offer the potential to advance health and health equity in the South over the long-term.
Key Themes from Roundtable Discussion
Health Insurance Coverage of the Low-Income Population
As in all regions, the ACA offers southern states the opportunity to increase coverage for the low-income population by expanding Medicaid to low-income adults and establishing Marketplaces for moderate-income individuals to obtain financial assistance for private coverage. States have options for implementing these coverage expansions. Specifically, as a result of the Supreme Court ruling on the ACA, the ACA Medicaid expansion to low-income adults was effectively made a state option. Regarding the Marketplaces, states may elect to create a state-based Marketplace, to use the federally-facilitated Marketplace, or to utilize a partnership model in which the state and federal government share roles and responsibilities. State implementation choices as well as outreach and enrollment efforts to connect eligible people to coverage will have important implications for health coverage in the region looking ahead.
New Coverage Options
Southern states have made varied implementation choices for the ACA coverage expansions. Some states in the region have fully embraced the coverage expansion opportunities under the ACA, expanding Medicaid and creating their own state-based Marketplaces. However, most southern states are using the federally-facilitated Marketplace and are not currently implementing the Medicaid expansion. Regardless of state implementation choices, the ACA provides opportunities to increase coverage by enrolling people in Marketplace coverage and enrolling those who were eligible under states’ previous Medicaid eligibility rules but not enrolled. Further, in states that expanded Medicaid, many low-income parents and other adults became newly eligible for the program. However, in states that have not implemented the Medicaid expansion, there is a gap in coverage for poor adults who remain ineligible for Medicaid but do not earn enough to qualify for the tax credits for Marketplace coverage, which begin at 100% of the federal poverty level.
Some southern states, such as Kentucky and Arkansas, pursued state-specific approaches to the ACA coverage expansions. Kentucky implemented the Medicaid expansion via executive order and built a state-based Marketplace. Employing lessons learned from implementation of the Children’s Health Insurance Program (CHIP), Kentucky used state-specific branding and marketing for its Medicaid and Marketplace coverage expansions. In Kentucky, all residents are directed to “Kynect, Kentucky’s Health Care Connection” for health coverage, and consumers generally do not view the new options for coverage as connected to the ACA or “Obamacare.” Participants indicate that the successful coverage expansion efforts in Kentucky have enabled the state to begin to focus on broader health goals, including improving access, meeting health care workforce needs, and advancing public health, for example, through reduced tobacco use. Arkansas pursued a state-federal partnership model for its Marketplace and obtained a waiver from the federal government to pursue a “private option” model for its Medicaid expansion so that individuals in the expansion receive subsidized coverage through the Marketplace. The state legislature must vote each year under budget rules to continue funding for the Medicaid expansion in Arkansas. As a result of continued political and ideological tensions over the expansion, the legislature recently passed new requirements for program changes in order for the Medicaid expansion to continue and imposed restrictions on assisters who help people enroll in coverage in the Marketplace.
For states that are not expanding Medicaid, the ACA still provides opportunities to improve coverage. Regardless of state decisions to expand Medicaid, people can still gain coverage through the new Marketplaces and under states’ existing eligibility rules. While experiences vary across states, recent data show that some southern states that have not expanded Medicaid have experienced significant enrollment increases since open enrollment for the new Marketplaces began, likely reflecting increased enrollment of people who were already eligible for the program due to outreach and enrollment efforts associated with the ACA and streamlined enrollment processes. However, participants noted that, in some southern states, advancing coverage has been challenging. Some states have reduced funding for outreach and enrollment efforts, threatening previous progress in expanding coverage, particularly for children, and some have imposed additional training requirements and limitations on enrollment assisters. However, stakeholders have been able to continue work quietly and achieve enrollment successes. In some cases, philanthropic organizations have provided funding to help assisters meet additional training requirements. Participants also indicated that, within states that are not politically supportive of the expansions, there still are opportunities to garner support for improved enrollment and retention policies under goals of good government and increased efficiency. Moreover, some states that have not adopted the Medicaid expansion are actively implementing other health care and health system improvements under the ACA and/or exploring alternative approaches to care for their low-income populations.
Outreach and Enrollment Efforts
Targeted and coordinated outreach and enrollment strategies have been key to reaching and enrolling eligible people in coverage. Many outreach and enrollment efforts associated with ACA implementation build upon lessons learned from the implementation of CHIP. Participants highlighted a wide range of outreach and enrollment strategies that have been utilized across the region, including conducting outreach through large community events such as the state fair and local sporting events, like football games; leveraging data from other programs, such as the Supplemental Nutrition Assistance Program (SNAP or food stamps), to facilitate enrollment; and drawing on resources from other policy areas—for example, using an incident command system for emergency preparedness to identify eligible populations. It was noted that provider visits also can provide a valuable opportunity to engage and enroll people in coverage, and certified enrollment assisters in hospitals and community clinics have achieved enrollment success. Providers’ role in enrollment varies though, as they are not all well-informed or well-positioned to enroll people in coverage. Overall, participants emphasized that coalition-building and coordination across entities have been central components of successful coverage efforts. However, sustaining enrollment networks as federal funding declines will be a primary challenge moving forward.
For hard-to-reach populations, including communities of color, it is important for outreach and enrollment efforts to come through trusted individuals within the community. There are a number of challenges to reaching these groups, including lack of knowledge and distrust and misperceptions about coverage options. In particular, fear and distrust stemming from restrictive immigration policies can hamper enrollment, particularly within the Latino community. Participants stressed that having champions within the community conduct outreach and enrollment and utilizing promotoras and other community health workers to reach out to eligible families can help reduce these enrollment barriers.
Addressing the needs of individuals who are left out of coverage because their state has not expanded Medicaid has been challenging for outreach and enrollment workers. Because many states in the South have not expanded Medicaid, a large share of people coming to enrollment events and completing applications with enrollment assisters fall into a coverage gap. These individuals have income too high to qualify for Medicaid but do not earn enough to qualify for premium subsidies for Marketplace coverage. Participants indicated that it has been difficult for assisters and individuals to invest time and effort in completing applications for individuals who are found ineligible for coverage because they fall into the gap. Enrollment assisters have found it helpful to connect individuals who fall into the gap to existing resources to address their current health care needs, and some assisters have developed lists of resources to provide to individuals in this situation.
Looking ahead
Achieving greater progress in expanding coverage within the region will require recognizing and working within the unique political dynamics of each state. Although there is wide variation in legislative structures and cultures across southern states, within all states in the region, politics are local and driven by a small group of primary influencers. Participants agreed that it will be necessary to understand and work within these state-specific dynamics and engage these primary influencers to achieve more progress in expanding coverage within the region. Some participants suggested it is valuable to encourage state legislators to “own” a problem and want to solve it, even if there is not agreement on a particular solution. Overall, documenting and sharing the lessons learned from southern states that are moving forward with the ACA coverage expansions will help inform and shape future coverage efforts in the region, recognizing that there is no deadline by which states must choose to expand Medicaid.
Health Care and the Safety-Net
To improve health outcomes in the long term, it also will be important to ensure that individuals are able to access needed primary and specialty care services. The ACA includes a number of provisions to help states improve health system capacity, including increased funding to expand community health centers and a temporary increase in Medicaid payment rates for primary care physicians. Increases in physician capacity will be especially important in areas with historically limited health resources, which include many areas in the South. Community health centers and other safety net providers will likely continue to serve an important role in providing care, especially for low-income and uninsured as well as rural populations. The continued and increased stress on safety-net providers may be particularly pronounced in the South, given that Medicaid eligibility for adults remains limited and the immigrant population is increasing. Overall, states in the South face a variety of challenges to improving access to care, and it will be important to build on successful initiatives and utilize existing resources and opportunities to address these challenges.
Increases in the availability of providers will be necessary to expand access to care. Participants stressed that broad workforce development efforts will be needed to establish sufficient provider capacity over the long term, particularly for primary care providers and within rural areas. In the shorter term, one potential opportunity to increase access to care in the region is to allow advanced practice nurses to practice at the top of their license. Southern states currently have some of the most restrictive practice limitations in the nation for nurse practitioners. Moreover, requirements for physician oversight of nurse practitioners can be problematic in rural areas in the region, as the nearest physician may be many miles away.
Hospitals may face increased strains on care capacity due to scheduled funding reductions and the absence of the Medicaid expansion in many states in the region. Disproportionate Share Hospital (DSH) payments, which help cover costs for hospitals that serve a large number of uninsured and Medicaid patients, are scheduled to be reduced under the ACA because it was anticipated that hospitals would serve fewer uninsured individuals as people gained coverage under the Medicaid expansion. These reductions were originally scheduled to go into effect on October 1, 2013, but were delayed until the beginning of fiscal year 2016, with double the reduction that would otherwise have applied that year. Allocations for the reductions have yet to be determined, but are legislatively required to take into account five factors, including a state’s uninsured rate. The scheduled DSH reductions would likely have a significant impact in the South, since many states in the region have not expanded Medicaid. Safety-net hospitals will continue to serve a large share of uninsured, low-income patients, especially in states with limited Medicaid coverage. Participants believe the reductions would likely lead to reductions in hospital clinical services and hospital closures, particularly among smaller rural hospitals that are already struggling to maintain their services and viability. To alleviate these impacts, some participants suggested that hospitals could explore options to redirect money flowing through other avenues and generate revenues by increasing enrollment of patients who are eligible for Medicaid under existing rules but not enrolled. However, even with mitigating efforts, the planned DSH reductions would likely have a significant negative impact on care capacity in the region. Although hospitals could be influential in encouraging states to expand Medicaid to minimize these consequences, some participants felt that engaging in the debate might put hospitals at risk for politically-driven cuts to other sources of state funding.
There is increased need for culturally and linguistically appropriate services given the growing diversity of the region. Participants indicated that strong beliefs in self-reliance and independence among some people in the rural community impede them from seeking care. As such, greater education about the value of obtaining regular care is necessary to ensure they access care appropriately. Participants suggested that establishing a diverse health care workforce to reflect the changing demographics of the population within the South will be an essential component of providing linguistically and culturally appropriate care and that achieving greater diversity among health professional leadership and faculty will be important for establishing a more diverse workforce over time.
There is a growing recognition of the importance of providing integrated physical and behavioral health care, and there are a number of promising initiatives underway to support integration. Participants emphasized that it will be necessary to promote integration at both the organizational level and the individual patient level. In particular, team-based care and provider training curricula that support team-based care (e.g., training interdisciplinary teams of doctors, nurses, social workers, etc.) were highlighted as potential strategies to support greater integration. Several successful integration initiatives are underway in the region, including collaborations between federally qualified health centers (FQHCs) and county mental health boards and care management and coordination initiatives for high-utilizers of the emergency room. Moving forward, participants suggested that striving to make integrated care the standard of care among safety-net providers will improve their ability to meet the high needs of the population they serve.
Aligning financial incentives will promote integration and coordination of care. Most current payment arrangements are tied to encounters and visits, rather than coordination or outcomes. Participants noted that tying payments to coordination and outcomes will facilitate greater integration and coordination of care and indicated that there has been greater movement toward pay-for-performance models within the region. However, it was recognized that some practices might not want to care for underserved populations that are sicker and more complex under these models, as they might negatively affect measures on which performance is assessed.
Health Equity and Public Health Outcomes
As noted, the South faces longstanding disparities in health, including greater prevalence of chronic conditions and worse health outcomes compared to other regions. Moreover, within the region, there are significant disparities by race and ethnicity. Moving the health care system away from a focus on treating sickness and disease to promoting wellness and prevention will facilitate greater equity and improvements in public health. There are a number of efforts in place at the federal level to reduce disparities, including new provisions under the ACA, as well as state and local level efforts. Overall, broad initiatives that extend beyond health care to address social determinants of health will be key for achieving progress in addressing the remaining challenges and gaps in health outcomes and equity within the region.
Southern states have improved some health outcomes over time, but significant challenges remain in achieving greater health equity. Participants recognized that the South has achieved some progress in improving health outcomes, and there has been notable improvement in the quality of care over the past decade. However, improvements in quality have not necessarily translated into increased health equity, and significant disparities remain. For example, although infant mortality rates in the region have fallen, rates still remain higher compared to other regions and marked racial and ethnic disparities persist, particularly between Whites and Blacks. Participants also noted that while there are fewer racial and ethnic disparities related to mental health, there are notable disparities between rural and urban populations. Moreover, mental health and substance use disorders are widespread and costly and can have spillover effects on the broader community. It was noted that serious substance use problems in one southern community impeded a company’s plans to expand jobs and operations in that area.
To advance health equity, efforts need to move beyond clinical services to address social determinants of health. Participants agreed that improving health and reducing disparities will require looking beyond medical care to address broader needs and challenges such as housing, transportation, food insecurity, and domestic violence. Some initiatives that seek to address broader needs are already underway in the region. For example, a new program in South Carolina performs a risk assessment of high need individuals, develops a plan to address their health and social needs, and then manages and coordinates their care. Yet, it remains challenging to implement approaches that integrate medical and social services, particularly given their different funding streams and bureaucracies. Looking ahead, participants suggested that it will be important to incorporate greater awareness of social determinants of health and community interventions into provider training and standards of care. It was noted that community health training components of nursing programs, which support more holistic care, offer valuable resources and opportunities that could help facilitate such efforts.
Increased data, broad and positive framing of issues, and identification of lessons learned from successful initiatives can help support reductions in disparities. Participants emphasized that the lack of adequate data currently available by race and ethnicity makes it challenging to measure progress in reducing disparities. Improvements in data collection and analytic capabilities are necessary to assess whether initiatives and activities are moving outcomes in the right direction and achieving greater equity. Participants also suggested that it is important to consider a broad range of potential interventions when seeking to reduce disparities, since the most effective solution to a problem may not be the direct inverse of its cause. Moreover, adopting positive framing for an issue rather than focusing on a problem can help garner increased support for improvement efforts—for example, focusing on the goal of saving babies’ lives rather than the problem of infant mortality. Lastly, participants suggested paths to success and lessons learned from successful initiatives can be applied to future efforts.
Health Care and the Economy
Overall, the ACA is anticipated to have broad economic impacts that will affect health care costs, state economies, jobs, and family budgets and spending. In particular, the Medicaid expansion is projected to increase state economic activity and have a positive effect on jobs and earnings. However, despite the economic arguments for expansion, many southern governors and legislators do not support the expansion due to concerns over state funding responsibilities for the program, competing economic demands, and political and ideological views.
Medicaid is an economic driver in state economies by bringing in federal matching dollars and supporting jobs. Medicaid is both an expenditure and a source of federal revenue in state budgets. The program is funded jointly by states and the federal government through a matching formula based on a state’s personal income and, in many southern states, where per capita personal income is less than the national average, the federal government pays at least two dollars for every dollar states spend on their programs. In all states that implement the Medicaid expansion, the federal government will pay an enhanced matching rate of 100% of the cost of coverage for newly eligible adults from 2014-2016, phasing down to 90% over time. Medicaid spending flows through a state’s economy, and the influx of federal funds magnifies the impact of state Medicaid spending. Medicaid funds directly support health care providers, including hospitals, community health centers, nursing facilities, group homes, and managed care plans. The funds also indirectly support other businesses and affect jobs, household spending, and state and local tax collections.
Several analyses of the potential impact of the Medicaid expansion in southern states have found that it would result in a net fiscal gain for states and increases in jobs, overall economic activity, and tax revenues. In Arkansas, projected revenue gains from the expansion led the state to implement tax cuts. Some participants suggested that that analyses of the potential impact of the Medicaid expansion fail to account for opportunity costs associated with the expansion, since spending in other areas (such as transportation) could increase federal funding and more directly increase jobs. Other participants felt that this argument does not apply to the Medicaid expansion because the federal funds are tied specifically to the expansion and 100% federal match in the early years.
Despite analyses projecting positive economic impacts, many southern governors and legislators do not support expanding Medicaid. Participants noted that those opposed to the expansion remain concerned about the state share of funding for the program over the long term and competing demands for state funds. Participants also indicated that political and ideological views continue to shape Medicaid expansion decisions in the region. It was noted that one of the main arguments some leaders in southern states have made against expanding Medicaid is that they do not want to direct more money into a broken system. Yet, some participants pointed out that many of these states are not fully utilizing options available to support improvement and innovation in the Medicaid program.
Challenges facing Medicaid are representative of challenges facing the larger health system. Participants had disparate views of the primary challenges facing Medicaid today. For example, while some believe Medicaid underpays providers, others view the program as more efficient than other types of coverage. However, there was general agreement among participants that many of the challenges facing Medicaid today are the same challenges facing the larger health care system, including demographic pressures (i.e., aging and disability), gaps in the supply and distribution of the health care workforce, and medical cost inflation. Given the significant role Medicaid plays in state health care systems, participants suggested that there are opportunities to leverage Medicaid at the state level to support broader health system transformation to address these system-wide issues.
Looking Ahead
In sum, the South is growing rapidly and experiencing demographic changes that have significant implications for health and health equity moving forward. The region’s health care system is in a transformational period as the ACA is implemented, and there is wide variation in how states in the region are addressing challenges and responding to opportunities to expand coverage and improve care that is framed in large part by the political and ideological context within each state.
The variation in state-level implementation of the ACA provides for natural experiments in the South as well as across the country. Participants noted that examining and tracking experiences in southern states such as Kentucky and Arkansas that are moving forward with Medicaid expansion, but in very different ways, will provide lessons for other states in the region and nationally. In both states, the ACA is being leveraged to support increases in health coverage as well as health care delivery system redesign and broader population health goals. Participants also suggested that it will be important to continue to track experiences in states that are not expanding Medicaid, and the degree to which they pursue alternative strategies to improve health care access and outcomes. Coverage options in the region may continue to evolve over time as there is no deadline by which states must decide to implement the Medicaid expansion. Moreover, states have the option to explore other state-specific coverage approaches when new state innovation waiver authority becomes available in 2017 that will allow states to waive Marketplace coverage provisions and combine those waivers with Medicaid, CHIP and other waivers. Regardless of state Medicaid expansion decisions, all states in the region are experiencing important changes in their health care systems under the ACA with new coverage opportunities available through the Marketplaces and modernized enrollment processes for Marketplaces and Medicaid. Moreover, many states are pursuing improvements in health care access and delivery systems.
As state actions and experiences in the region unfold, understanding their implications for racial and ethnic as well as geographic disparities in the region will be key. Participants emphasized that to improve health and health equity in the region, it will be important to identify clear goals and measure progress, particularly given its unique geography, demographics, and challenges. They noted that advancing these goals will require a long-term strategy that looks beyond traditional leadership models and health care-focused approaches. Building partnerships that tap into community assets and leverage trusted community leaders and coalitions will be essential for engaging populations and establishing the community infrastructure necessary to provide everyone with opportunities to lead healthy lives. In addition, participants suggested that aligning policies aimed at improving health with efforts to address the social determinants of health, such as housing, education, food security, and employment, will facilitate broad improvements over time.