2016 Employer Health Benefits Survey
Section Nine: Prescription Drug Benefits
Almost all covered workers have coverage for prescription drugs. For 2016, to reduce burden on respondents, we revised the survey to ask respondents about the attributes of prescription drug coverage only in their largest health plan; previously, we asked about prescription coverage in their largest plan for each of the plan types that they offered. In addition, we began asking employers about their cost sharing for tiers that cover specialty drugs exclusively. In cases in which a tier covers only specialty drugs, we report the plan attributes under the specialty banner, rather than as one of the four standard tiers. Therefore, the number of tiers a firm reports may not correspond with the number of tiers for which we have cost-sharing information. For more information, see the survey design and methods section. While this new approach produces estimates that are quite similar to those obtained by the prior method, we do not do statistical comparisons with 2016 estimates and those from prior years.1
- Nearly all (more than 99%) covered workers work at a firm that provides prescription drug coverage in their largest health plan.
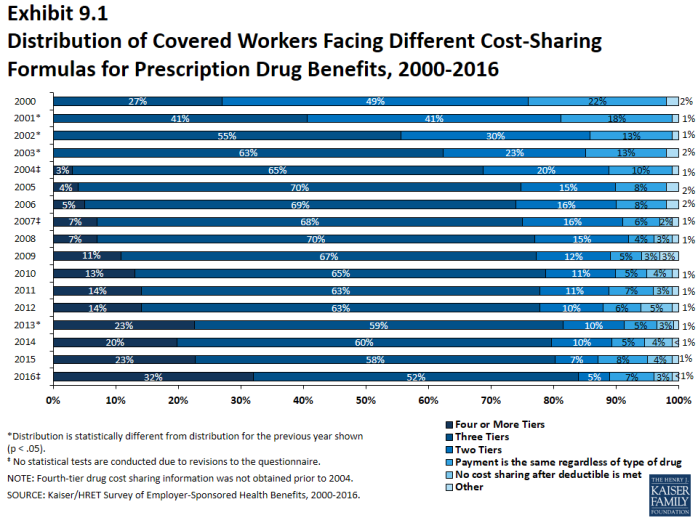
- A large share of covered workers (89%) work at a firm whose largest health plan has a tiered cost-sharing formula for prescription drugs (Exhibit 9.1). Cost-sharing tiers generally refer to a health plan placing a drug on a formulary or preferred drug list that classifies drugs into categories that are subject to different cost sharing or management. It is common for there to be different tiers for generic, preferred and non-preferred drugs. In recent years, plans have created additional tiers which, for example, may be used for lifestyle drugs or expensive biologics. Some plans may have multiple tiers for different categories; for example, a plan may have preferred and non-preferred specialty tiers. The survey obtains information about the cost-sharing structure for up to five tiers.
- Eighty-four percent of covered workers work at a firm that has three, four, or more tiers of cost sharing for prescription drugs in their largest health plan (Exhibit 9.1).
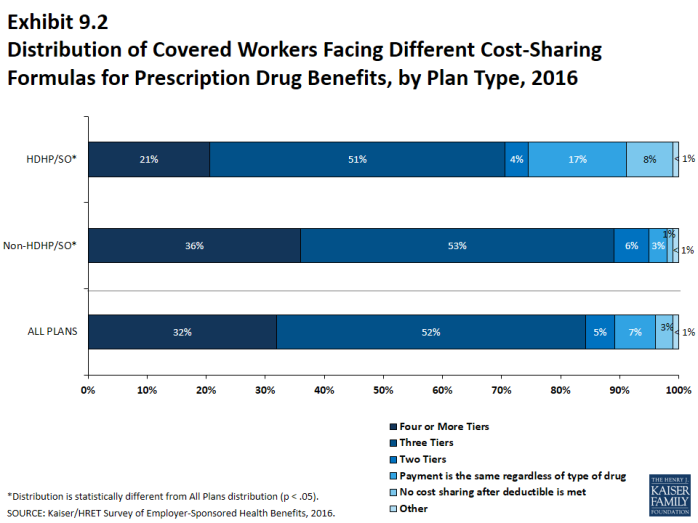
- Covered workers at large firms (200 or more workers) whose largest health plan is an HDHP/SO have a different cost-sharing pattern for prescription drugs than covered workers with other plan types: they are more likely to be in a plan with the same cost sharing regardless of drug type (17% vs. 3%) or in a plan that has no cost sharing for prescriptions once the plan deductible is met (8% vs. <1%) (Exhibit 9.2).
Three or More Tiers
- Thirty-two percent of covered workers work at a firm whose largest health plan has four or more tiers of cost sharing for prescription drugs (Exhibit 9.1).
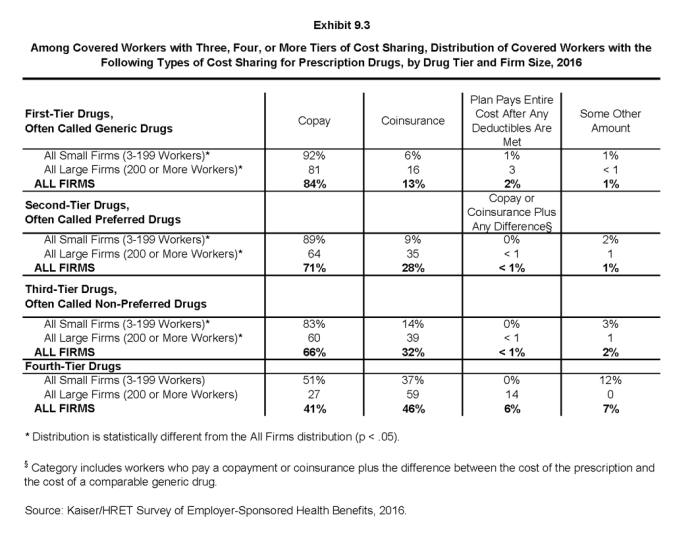
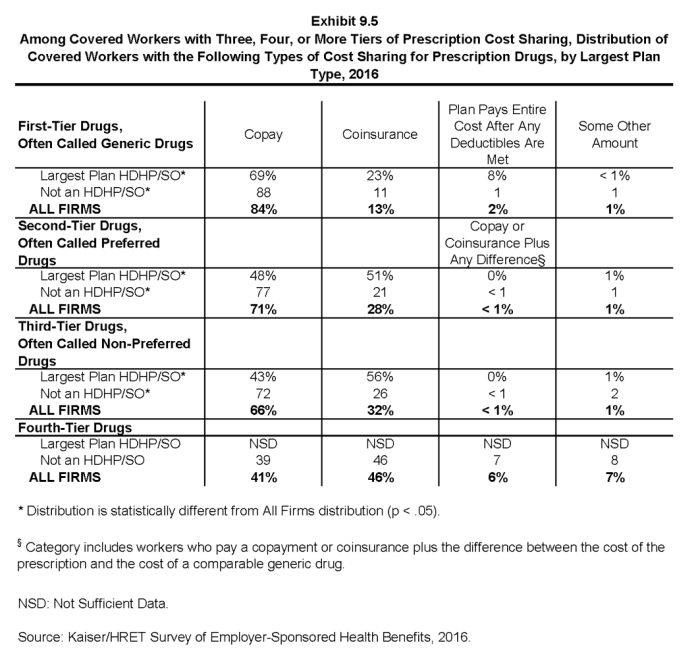
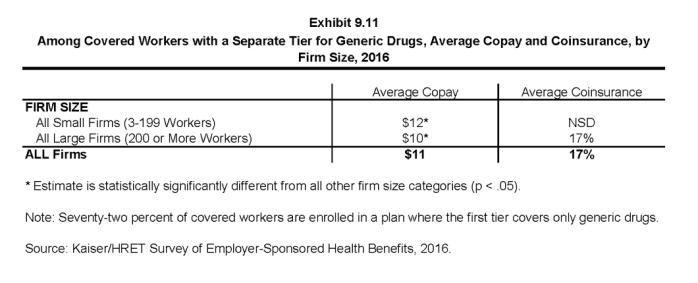
- For covered workers at firms whose largest plan has three or more tiers of cost sharing for prescription drugs, copayments are the most common form of cost sharing in the first three tiers and coinsurance is the next most common. Among those with a fourth tier, 46% have a coinsurance requirement and 41% have a copayment (difference not significant) (Exhibit 9.3).
- Among covered workers at firms whose largest health plan has three or more tiers of cost sharing for prescription drugs, the average copayments are $11 for first-tier drugs, $33 second-tier drugs, $57 third-tier drugs, and $102 for fourth-tier drugs (Exhibit 9.4).
- Among covered workers at firms whose largest health plan has three or more tiers of cost sharing for prescription drugs, the average coinsurance rates are 17% for first-tier drugs, 25% second-tier drugs, 37% third-tier drugs, and 29% for fourth-tier drugs (Exhibit 9.4).
Single and Two Tiers
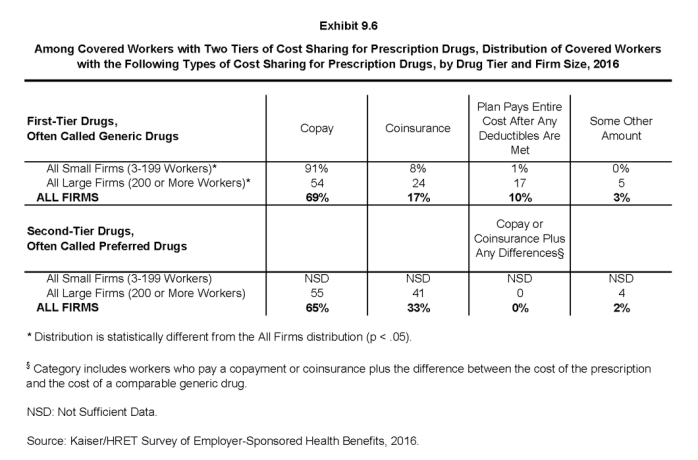
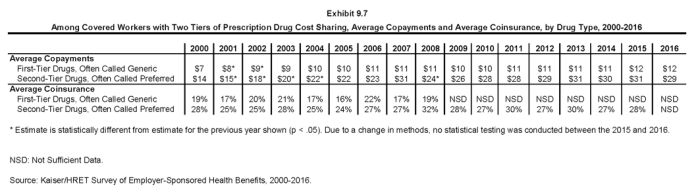
- Five percent of covered workers work at firms whose largest health plan has two tiers for prescription drug cost sharing (Exhibit 9.1). For these workers, copayments are more common than coinsurance for both first-tier and second-tier drugs. The average copayment for the first tier is $12 and the average copayment for the second tier is $29 (Exhibit 9.7).
- Seven percent of covered workers at firms whose largest health plan covers prescription drugs have the same cost sharing regardless of the type of drug (Exhibit 9.1).
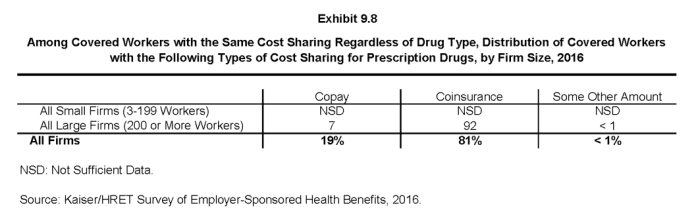
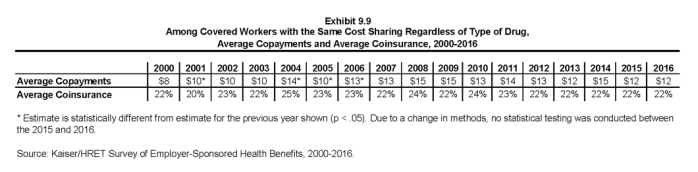
- Among these workers, 19% have copayments and 81% have coinsurance (Exhibit 9.8). The average coinsurance rate is 22% and the average copayment is $12 (Exhibit 9.9).
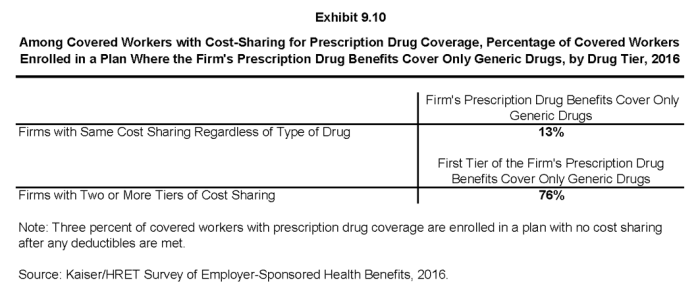
- Thirteen percent of these workers are at firms whose largest health plan limits coverage for prescriptions to generic drugs (Exhibit 9.10).
Limits on Coinsurance
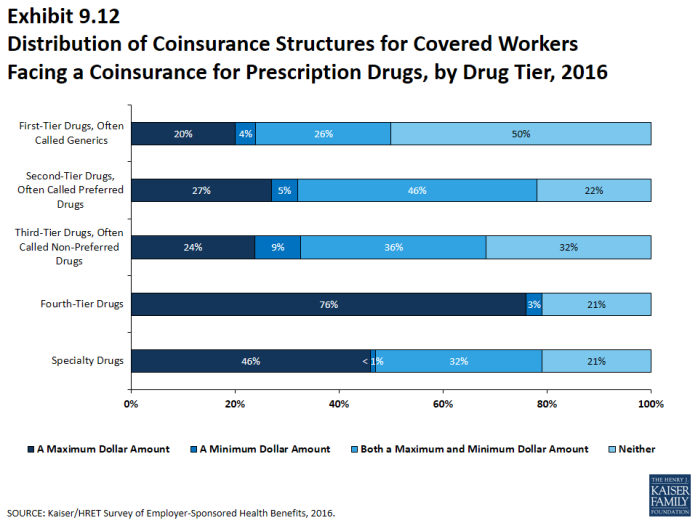
- Coinsurance rates for prescription drugs often have maximum and/or minimum dollar amounts associated with the coinsurance rate. Depending on the plan design, coinsurance maximums may significantly limit an enrollee’s out-of-pocket spending on higher cost drugs.
- These coinsurance minimum and maximum amounts vary across the tiers. Among covered workers at firms whose largest health plan has coinsurance for the first cost-sharing tier, 20% have only a maximum dollar amount attached to the coinsurance rate, 4% have only a minimum dollar amount, 26% have both, and 50% have neither. For those with coinsurance for the fourth cost-sharing tier, 76% have a maximum dollar amount, 3% have a minimum dollar amount, and 21% have neither (Exhibit 9.12).
Specialty drugs
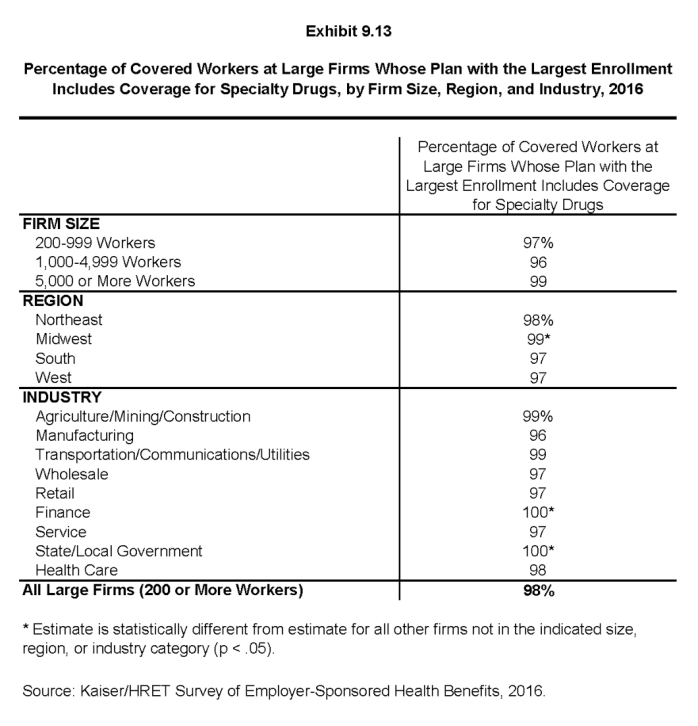
- Specialty drugs such as biologics may be used to treat chronic conditions and often require special handling and administration. We revised the questions in the 2016 survey regarding specialty drugs, and are reporting results only among large firms because a large share of small firms were unsure whether their largest plan covered these drugs.
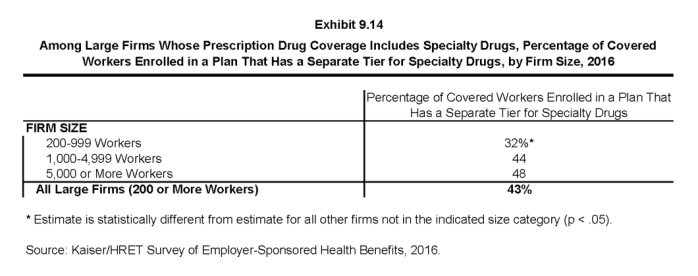
- Ninety-eight percent of covered workers at large firms work for employers whose largest health plan provides coverage for specialty drugs (Exhibit 9.13). Among these workers, 43% work at firms whose largest plan has a cost-sharing tier just for specialty drugs (Exhibit 9.14).
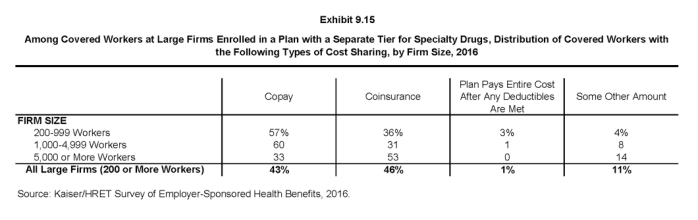
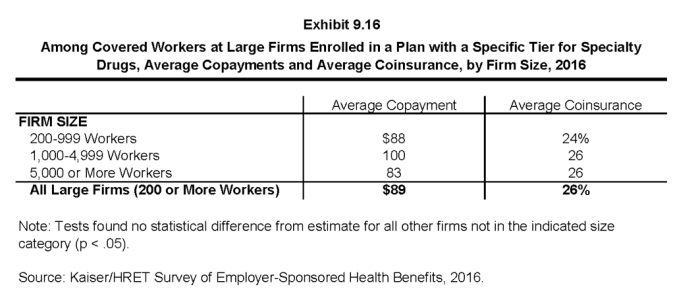
- Among covered workers at large firms whose largest plan has a separate tier for specialty drugs, 43% have a copayment for specialty drugs and 46% have a coinsurance requirement (Exhibit 9.15). The average copayment is $89 and the average coinsurance rate is 26% (Exhibit 9.16). Seventy-eight percent of those with a coinsurance requirement have a maximum dollar limit on the amount of coinsurance they must pay.
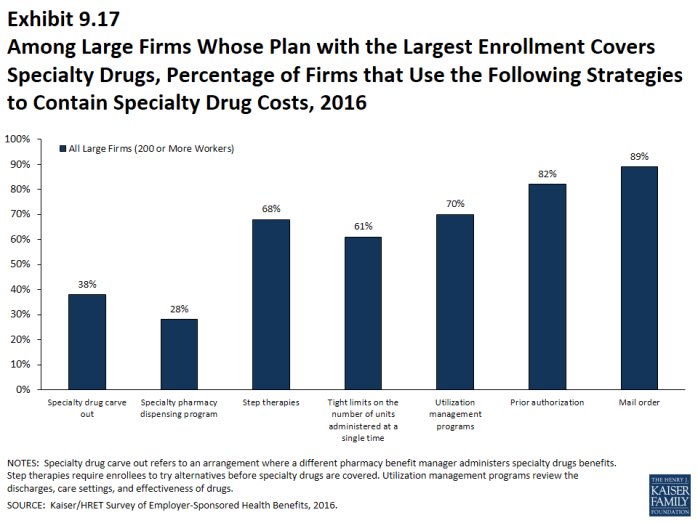
- Specialty drugs are typically high cost; firms use a variety of strategies to contain these costs. Among covered workers at large firms whose largest health plan provides coverage for specialty drugs, 38% use a different pharmacy benefit manager for specialty drugs; 28% have a dispensing program with incentives to encourage enrollees to receive specialty drugs in an alternative setting; 68% use a step therapy approach where enrollees must try alternatives before specialty drugs are covered; 61% use tight limits on the number of units administered at a single time; 70% use utilization management programs to review discharges, care settings and effectiveness; 82% require prior authorization; and 89% have a mail order option for specialty drugs (Exhibit 9.17).2
Generic drugs: Drugs product that are no longer covered by patent protection and thus may be produced and/or distributed by multiple drug companies.
Preferred drugs: Drugs included on a formulary or preferred drug list; for example, a brand-name drug without a generic substitute.
Non-preferred drugs: Drugs not included on a formulary or preferred drug list; for example, a brand-name drug with a generic substitute.
Fourth-tier drugs: New types of cost-sharing arrangements that typically build additional layers of higher copayments or coinsurance for specifically identified types of drugs, such as lifestyle drugs or biologics.
Brand-name drugs: Generally, a drug product that is covered by a patent and is thus manufactured and sold exclusively by one firm. Cross-licensing occasionally occurs, allowing an additional firm to market the drug. After the patent expires, multiple firms can produce the drug product, but the brand name or trademark remains with the original manufacturer’s product.