Building on the Evidence Base: Studies on the Effects of Medicaid Expansion, February 2020 to March 2021
Themes in Recent Research
Several key themes emerge from recent literature investigating the effects of Medicaid expansion (Figure 1). In contrast to earlier research, which largely focused on the impacts of Medicaid expansion for the general population or for low-income populations, recent research has increasingly focused on outcomes for specific populations, such as people with cancer or behavioral health needs. Recent research has also focused on specific outcomes such as mortality and social determinants of health. Although overall findings across these themes generally show positive effects of Medicaid expansion, a smaller number of studies find no impact of expansion on specific outcomes for specific populations; however, very few studies suggest any negative effects.
Many studies published between February 2020 and March 2021 and cited throughout this report have findings across multiple of these themes and are thus cited in multiple sections. Additionally, many studies on expansion published prior to February 2020 also have findings related to these themes but are not cited in this report; however, these can be found cited in an earlier literature review and are also included in the Bibliography and Appendices to this report.
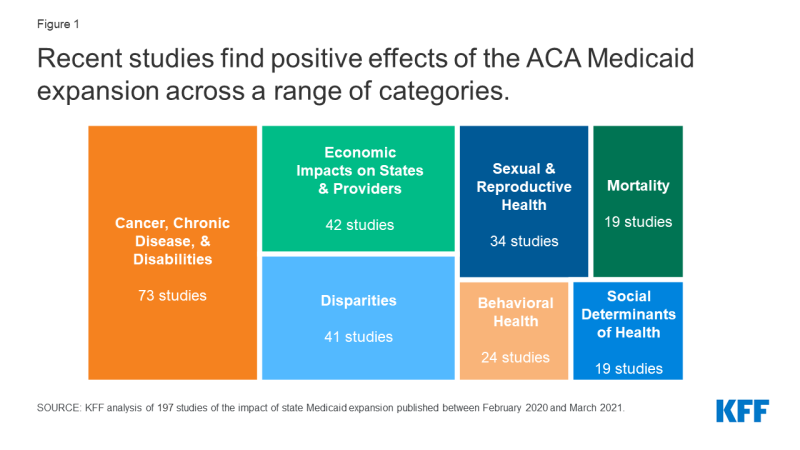
Figure 1: Recent studies find positive effects of the ACA Medicaid expansion across a range of categories.
Mortality
A growing body of research finds that Medicaid expansion has improved overall mortality rates as well as mortality rates associated with some specific health conditions. These findings are consistent with earlier research identifying that expansion contributed to declines in overall and some specific mortality rates, but had no effect on mortality rates associated with other specific conditions.
- Overall mortality. A 2020 national study found that expansion was associated with a significant 3.6% decrease in all-cause mortality, the majority of which was accounted for by a significant 1.93% decrease in health care amenable mortality. Another study found that expansion was associated with reductions in health care amenable mortality and in mortality not due to drug overdose.1,2
- Mortality associated with specific health conditions. A larger number of studies consider the impact of expansion on mortality rates for particular populations or associated with certain health conditions:
- Studies find that expansion was associated with significant declines in mortality related to certain specific conditions, in some instances limited to certain subgroups. These findings include decreased mortality associated with different types of cancer, cardiovascular disease, and liver disease. Studies also find decreased maternal mortality, and one study found a decrease in infant mortality among Hispanics only.3,4,5,6,7,8,9,10
- However, other studies suggest no effect of expansion on mortality among safety-net hospital patients, individuals with glottic cancer, individuals with glioblastoma, patients undergoing hemodialysis, and overall infant mortality. One study found no significant difference between COVID-19 mortality rates in expansion versus non-expansion states, despite lower incidence rates in expansion states. One study concluded that available data was insufficient to adequately identify the impact of expansion on opioid mortality.11,12,13,14,15,16,17,18,19
Cancer, Chronic Disease, and Disabilities
Recent research finds largely positive impacts of expansion on coverage and access to care among populations with cancer, chronic disease, and/or disabilities. However, findings on utilization of care and health outcomes are more mixed, with some studies suggesting improvements and others finding no effect of expansion. These studies build on prior research indicating generally positive effects of expansion for populations with cancer and other health conditions. Recent research also provides additional evidence on expansion’s impacts across a range of chronic conditions considered by the CDC to put people at higher risk of severe illness and death from COVID-19 (such as diabetes, obesity, and lung and heart conditions).
- Cancer. A large body of recent research considers the impact of Medicaid expansion on coverage, treatment, and outcomes of people with cancer, as well as access to cancer screenings.
- Coverage of people with cancer. Studies overwhelmingly find that Medicaid expansion has increased insurance coverage rates among cancer patients and survivors. Research also finds changes in payer mix of care for patients with cancer, with declines in the proportion of uninsured patients and increases in the proportion of Medicaid-insured patients.20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43
- Cancer diagnosis, treatment, and outcomes. Most studies find an association between expansion and increases in early-stage diagnosis rates among cancer patients, suggesting that expansion has facilitated earlier utilization of care for these patients. Findings on utilization of cancer treatment services and on access to timely treatment are mixed, though more studies find improvements as compared to studies that find no effect of expansion. Of studies that consider cancer mortality, three suggest improvements for patients with certain types of cancer, while three suggest no effect for patients with other types of cancer.44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75
- Cancer screening and prevention. Several studies find that expansion increased receipt of cancer screenings such as mammograms, though a similar number of studies find no effect of expansion on screening rates for certain cancers. Two studies identified an association between expansion and increased rates of human papillomavirus (HPV) vaccines (overall and among teenagers specifically), while a third found no effect of expansion on HPV vaccination rates among female community health center patients.76,77,78,79,80,81,82,83,84
- Diabetes. Studies find that expansion increased insurance coverage rates among adults and teenagers with diabetes. Although research indicates that expansion increased affordability of health care for populations with diabetes, findings on utilization of preventive care and treatment are more mixed (between studies finding improvements and studies finding no effect). Two studies identified improvements in diabetes biomarkers among community health center patients following expansion. Two studies that considered women of reproductive age found that expansion did not affect the prevalence of diabetes prior to or during pregnancy.85,86,87,88,89,90,91,92,93,94,95,96
- Other chronic disease. In addition to cancer and diabetes, research also considers a range of other chronic conditions including cardiovascular and pulmonary diseases, obesity, and liver disease. Studies find that among those with chronic disease, expansion contributed to increased insurance coverage and improvements in payer mix, improved access to care, and better health outcomes including disease management and mortality. Findings on effects on treatment utilization and quality of care were mixed (between studies finding improvements and studies finding no effect). Finally, studies generally suggest that expansion increased screening for chronic conditions but did not reduce the prevalence of these conditions except for smoking.97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123
- People with disabilities. A small number of recent studies consider the impacts of expansion for people with disabilities. One study found increased coverage options for people with disabilities in expansion states, while other studies suggested no effect of expansion on utilization of care or employment among this population. One study found that expansion improved mental health outcomes for caregivers of people with disabilities.124,125,126,127,128
Sexual and Reproductive Health
Recent research finds that expansion has contributed to improvements in a number of outcomes related to sexual and reproductive health. This body of research includes findings related to women’s health and HIV/AIDS outcomes, both areas of health care that have faced increased challenges during the coronavirus pandemic. Building on prior research finding positive impacts among people of reproductive age, recent research indicates that expansion has improved measures including coverage rates before, during, and after pregnancy; maternal mortality and infant health outcomes; utilization of the most effective contraceptive methods; and screening for HIV/AIDS.
- Maternal and infant health outcomes. Studies find that expansion significantly increased access to and utilization of health care for pregnant women and mothers. Two studies found significant declines in maternal mortality, in contrast to one study which found no impact of expansion on certain health outcomes during pregnancy. Studies generally suggest an association between expansion and improvements in birth outcomes such as low birthweight, but find no impact on infant mortality (except for one study which found a reduction in Hispanic infant mortality only).129,130,131,132,133,134,135,136,137,138,139,140
- Postpartum insurance coverage. Although the American Rescue Plan Act of 2021 created a new option to expand postpartum coverage to 12 months via a State Plan Amendment, current federal statute requires that pregnancy-related Medicaid coverage continue through just 60 days. Research indicates that ACA Medicaid expansion has decreased coverage loss after this 60-day period ends: all recent studies that consider rates of insurance coverage after pregnancy find that expansion significantly increased postpartum coverage. Studies also suggest an association between expansion and increased coverage prior to and during pregnancy.141,142,143,144,145,146,147,148,149
- Access to contraception. Most studies find that expansion increased utilization of the most effective contraception methods (long-acting reversible contraception, which includes IUDs and implants); however, studies generally find no effect on overall contraception use. One study found an association between expansion and improved payer mix for contraceptive visits at safety net clinics, with a decline in the proportion of uninsured patients and an increase in the proportion of publicly-insured patients.150,151,152,153,154,155
- HIV/AIDS screening and outcomes. Studies suggest that expansion increased overall rates of HIV screening, including one study that found that increases in HIV test and diagnosis rates occurred despite no change in actual HIV incidence. Research also indicates higher insurance coverage rates among people with or at risk of HIV, increased utilization of Pre-Exposure Prophylaxis (PrEP) to treat HIV, and improved quality of care for patients with HIV.156,157,158,159,160,161,162,163,164,165,166,167
Behavioral Health
A growing body of research finds that expansion is associated with improvements in access to care and outcomes related to substance use disorder (SUD) as well as other mental health care. These findings are consistent with prior research indicating positive effects of expansion on behavioral health care access and outcomes. Recent research on SUD largely focuses on opioid use disorder (OUD) specifically, which is more prevalent among Medicaid enrollees as compared to the general population. Given the impacts of the coronavirus pandemic on mental health and substance use, Medicaid expansion coverage is likely to continue to serve as a significant source of coverage for behavioral health care.
- Access to care and outcomes for SUD. Studies find that Medicaid expansion was associated with increased insurance coverage among adults with SUD and improved payer mix of SUD-related visits (declines in uninsured patients and/or increases in Medicaid-covered patients). Studies also find that expansion increased the receipt of medication assisted treatment (MAT) prescriptions for the treatment of OUD, and that following expansion opioid treatment facilities were more likely to offer MAT and comprehensive mental health services. In contrast, a small number of studies found no effect of expansion on utilization of certain health care services for SUD. One study found no effect of expansion on drug-overdose deaths, while a second concluded that available data was insufficient to adequately identify the impact of expansion on drug-related mortality.168,169,170,171,172,173,174,175,176,177,178,179,180,181
- Mental health care access and outcomes. Studies find that expansion increased access to care for adults with mental health conditions such as depression, including by increasing the likelihood that mental health care providers accepted Medicaid. Findings on utilization of mental health care are more mixed, with some studies suggesting increased utilization of services such as mental health care via telehealth, and others finding no effect of expansion on other mental health services. Findings on mental health outcomes are also mixed: one study found that expansion was associated with improvements in self-reported mental health among low-income adults, while two other studies found no impact on similar measures among near-elderly adults and among women of reproductive age.182,183,184,185,186,187,188,189,190,191,192,193
Economic Impacts on States and Providers
Building on prior research, recent studies identify positive financial impacts of Medicaid expansion for states, hospitals, and other providers. These studies join a body of prior research finding overwhelmingly positive effects of expansion on economic outcomes (see Appendix A, Figure 5). These economic findings are particularly relevant given fiscal stress experienced by both states and Medicaid providers during the coronavirus pandemic.
- State budgets and economies. All recent studies that consider the financial impacts of expansion for states find positive effects. Studies find that expansion states experienced increased federal Medicaid spending. One study found that through 2018, Medicaid expansion led to increased federal spending in expansion states but very small (<1%), insignificant increases in spending from state sources (including in 2017 and 2018 when states began paying 5% and 6% of expansion costs respectively, a rate that was subsequently phased to 10% in 2020 and beyond). In addition, Medicaid expansion did not crowd out other areas of state spending and states that did not expand passed up $43 billion in federal funds in 2018. Research also finds that expansion resulted in increased revenue as well as net state savings by offsetting state costs in other areas, such as state spending on substance use disorder (SUD) treatment and on the traditional Medicaid program. One study found that the mortality reductions associated with expansion resulted in between $20.97 and $101.8 billion in annual welfare gains, implying that mortality-related savings alone may offset the entire net cost of expansion.194,195,196,197,198
- Payer mix. Studies overwhelmingly find that Medicaid expansion has resulted in payer mix improvements (declines in uninsured patients and/or increases in Medicaid-covered patients). Findings include payer mix improvements for hospitalizations, emergency department visits, and visits to community health centers and other safety-net clinics. Studies identify payer mix improvements among patients hospitalized for a range of specific conditions including traumatic injuries, surgeries, and treatment for substance use disorder. In line with payer mix improvements, studies also find decreased uncompensated care costs (UCC) overall and for specific types of hospitals, including those in rural areas.199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227,228,229,230
- Financial performance of hospitals and other providers. Research finds that expansion contributed to increased hospital revenue overall and from specific services. Although studies find that expansion has improved provider operating margins and profitability, these findings vary by hospital type. For example, one study found that despite declines in UCC and increases in Medicaid revenue across all hospital types, only hospitals in non-metropolitan areas and small hospitals experienced improved profit margins; another study similarly found gains in overall revenue only for rural and small hospitals. A few studies suggest that improvements in payer mix and UCC at hospitals may have been partially offset by increases in unreimbursed Medicaid care and declines in commercial revenue. One recent study found that expansion reduced the number of annual hospital closures.231,232,233,234,235,236,237,238,239,240,241
Disparities
A growing body of research considers the impact of Medicaid expansion on disparities in different outcomes by race/ethnicity, socioeconomic status, and other categories. These studies build on an earlier literature review finding that expansion has helped to narrow racial disparities in coverage and certain health outcomes, with more limited evidence suggesting reduced racial disparities in access to and use of care. Some studies on racial/ethnic disparities cited here are also included in this earlier review, which included studies published through July 2020.
- Disparities by race/ethnicity. Findings on expansion’s impact on racial disparities in health coverage, access, and outcomes are mixed and generally mirror findings from a previous literature review, with evidence of decreased racial disparities for some populations in measures including coverage rates, affordability of care, utilization of surgery and other services, and health outcomes including maternal and infant mortality. However, similar numbers of studies identify no effect of expansion on racial disparities in these and other measures. A very small number of studies find evidence of increased racial disparities (in coverage rates for specific populations and in breast cancer mortality). Across outcomes, most research focuses on disparities for Black and Hispanic individuals, with limited findings on impacts for other groups of color.242,243,244,245,246,247,248,249,250,251,252,253,254,255,256,257,258,259,260,261,262,263,264,265,266,267,268,269,270,271,272,273,274,275,276,277,278,279,280
- Disparities by socioeconomic status (income and/or education). In contrast to research on racial disparities, recent studies that consider socioeconomic disparities all find improvements. Studies find that expansion has reduced disparities in coverage by income and/or education status, including for populations with certain cancer diagnoses. A smaller number of studies also find decreased socioeconomic disparities in utilization of care, certain health outcomes such as maternal mortality, and individual financial stability.281,282,283,284,285,286,287,288,289,290,291
- Disparities by other categories. A few recent studies identify an association between expansion and reduced coverage disparities by age, sex, and marital status, but no effect on coverage disparities by work status and obesity. One study found that expansion reduced age disparities in individual financial stability. Another study found no effect of expansion on disparities by sex in receipt of HIV tests.292,293,294,295,296,297,298
Social Determinants of Health
Recent research indicates largely positive impacts of expansion associated with different social determinants of health. These recent studies are consistent with prior research on expansion’s effect on social determinants of health and also contribute new evidence on effects for certain measures. Social determinants of health are the conditions in which people are born, grow, live, work, and age. Improvements in these measures associated with expansion could help to mitigate increased hardship due to the coronavirus pandemic.
- Access to care in rural areas. Studies find that expansion was associated with greater improvements in access to care in rural areas, including increased HIV diagnosis rates and access to mental health care. In contrast, one study found that utilization of tobacco cessation treatment remained limited in rural Appalachia even after Medicaid expansion in Kentucky. Research also suggests that rural hospitals experienced particularly substantial improvements in financial performance following expansion.299,300,301,302,303,304,305,306,307
- Impacts on economic stability, employment, and educational outcomes. Studies find that expansion decreased catastrophic health expenditures (health care spending as a percentage of family income). One study found that expansion was associated with greater increases in income among low-income individuals and contributed to decreased levels of income inequality. One study found an association between expansion and decreased odds of job loss, though two other studies found no effect of expansion on employment among people with disabilities. Finally, a national study found significant reductions in high school dropout rates in the first year of expansion implementation, which would translate to an 11.2% reduction in drop-out rates in non-expansion states if they adopted the expansion.308,309,310,311,312,313,314
- Outcomes for justice-involved and individuals experiencing homelessness. One study found that although pregnant women referred by criminal justice agencies to opioid use disorder (OUD) treatment facilities received medication as treatment at lower rates than women referred by other sources, expansion mitigated this effect by increasing receipt of medication for these women. Another study found that expansion resulted in decreased rates of recidivism in some geographic areas. A study in Arkansas found a spike in utilization of acute care among adults experiencing homelessness who gained coverage through expansion, suggesting a pent-up demand that stabilized in the years following expansion implementation.315,316,317
Looking Ahead
This literature review builds on a prior report and summarizes new evidence on more specific outcomes for certain populations. The full body of Medicaid expansion research includes over 600 studies (summarized in Appendix A) and indicates overall positive effects across a range of outcomes for patients, providers, and states. These findings suggest that Medicaid expansion could help mitigate adverse impacts of the coronavirus pandemic at the patient, provider, and state level; although research to date on Medicaid expansion and COVID-19 remains limited, future studies will likely further consider these impacts. Additionally, continued research cited in this report demonstrating positive economic impacts may help inform states still debating whether to adopt the expansion, particularly given the new ARPA financial incentive that would more than offset state expansion costs for two years (after which states would continue to bear 10% of the cost). Future policy proposals at the state and federal level could further affect Medicaid expansion coverage and options for people in the coverage gap.
The authors thank Diana Park for her assistance reviewing studies for inclusion and compiling supplemental materials.
