Implementation of the ACA in Kentucky: Lessons Learned to Date and the Potential Effects of Future Changes
What has been Kentucky’s ACA implementation experience to date?
Kentucky has had one of the most successful ACA implementation experiences among states. Beginning in 2014, the state expanded Medicaid to low-income adults and built its own State-Based Marketplace, kynect. Since implementing the ACA, Kentucky’s uninsured rate fell from 16% in 2013 to 8% in 2014, one of the largest reductions in the country.1 Much of this reduction is attributed to the Medicaid expansion. Total enrollment in Medicaid grew by over 570,000 or 94% from the pre-ACA baseline period of July – September 2013 to December 2015.2 As of December 2015, the program covered roughly a quarter of the state’s population. Nearly 94,000 people are enrolled in coverage through kynect, which represents about 38% of the potential Marketplace population.3
Several components have contributed to Kentucky’s success implementing the ACA, including strong leadership and collaboration; a high-functioning integrated eligibility system for Medicaid and Marketplace coverage; broad outreach and marketing efforts; a robust and diverse network of enrollment assistance; and initiatives to strengthen access to care for Medicaid enrollees as more individuals enroll as discussed below.
Leadership and Collaboration
Stakeholders reported that kynect and Medicaid officials were highly engaged and personally committed to achieving success and were often present at outreach and enrollment events. The previous Governor made successful implementation of the coverage expansions in 2014 a priority, and this leadership carried down through state officials. Many of the state agencies involved in health reform implementation, including Medicaid, kynect, and the Department for Community Based Services, are peer agencies housed within the Kentucky Cabinet for Health and Family Services. Stakeholders indicated that this structure helped promote strong working relationships among the agencies and that they worked hand-in-hand throughout planning and implementation of the coverage expansions. There was also close coordination between kynect and the Department of Insurance. Further, the state engaged with other stakeholders early and often, including the community, advocates, assisters, agents, and providers.
“We have weekly stakeholder meetings over at kynect. It gets us all in a room and it’s a lot harder to fuss when you’re looking at somebody because we’re all peer agencies. We’re all under the same umbrella but it’s easy to get frustrated. If you all get in a room once a week it’s hard to stay frustrated because you just ask the questions and work through things. I think they’ve been very effective.”—Medicaid official
Eligibility System
One of the most pivotal components of Kentucky’s enrollment success is the single, integrated eligibility system it built for kynect and Medicaid. When the ACA coverage expansions took effect in January 2014, Kentucky launched a new integrated eligibility system that made eligibility determinations for both kynect Marketplace coverage and for non-disabled Medicaid groups, including children, pregnant women, parents and adults newly eligible through the ACA Medicaid expansion. While the Federally-Facilitated Marketplace (FFM), Healthcare.gov, and most State-Based Marketplaces experienced large system problems during the initial year of implementation in 2014, Kentucky was one of the few states that had a largely successful system launch. This successful system launch facilitated streamlined enrollment of eligible individuals in both kynect and Medicaid coverage.
Stakeholders point to a number of factors that contributed to the state’s system success. One key component is that it is a fully integrated system, which eliminates the need to transfer data between kynect and Medicaid. Moreover, consumers only receive a single notice of their determination rather than separate notices from each program, minimizing confusion. At its outset, the system also was able to make real-time determinations for most cases and could handle complex situations in which members of a family may be eligible for different types of coverage. The system also included features that consumers valued, such as a pre-screen feature that allowed consumers to anonymously shop for coverage after answering a few quick questions, as well as the ability to electronically upload documentation when it is required.
“It’s a one stop shop. You know, it takes maybe 30 to 45 minutes. You enter your information. If you’re Medicaid eligible, you pick a Medicaid managed care organization. If you’re QHP eligible, you pick a qualified health plan. So, certainly that one stop shop streamlined application process I think really contributed to our success.” –kynect official
The system’s success was underpinned by the state’s close work with contractors, ongoing implementation of workarounds and incremental fixes as needed, and use of data and feedback loops to identify problems. Stakeholders stressed that close collaboration among policy staff, IT systems staff, and contractors was vital during both the initial build of the system and on an ongoing basis to manage the system and quickly resolve problems. Contractors were co-located on site with state policy and IT staff to facilitate close and constant communication. Stakeholders also noted that the state would implement workarounds and incremental fixes when it faced early problems or glitches with its system, which allowed for continuous improvement. Medicaid and kynect officials also pointed to the importance of using data and feedback loops to understand how the system was functioning and identify problems. During the initial launch, officials reported that they closely tracked statistics to monitor system operations and would target fixes or changes as necessary when the data pointed to problems.
The state continued to refine and enhance the system over time. The system did face some early technological glitches, but stakeholders generally agreed that many were resolved by the end of the first open enrollment period. The state implemented several enhancements to the system prior to the second open enrollment period. These enhancements included allowing consumers to see premium costs with the advance premium tax credits applied when shopping for plans. In addition, the system was adjusted to display silver plans at the top of the plan list for people who qualify for cost-sharing reductions, given that these plans have the best value for these consumers by providing access to the cost-sharing reductions. Stakeholders reported that the system functioned very smoothly during the second open enrollment period, which allowed more individuals to self-enroll and freed up assistance resources to address more complex cases. As of the end of the second open enrollment period, the state was planning for continued improvements and enhancements, including addressing system problems affecting enrollment for immigrants and refugees and consumers changing plans at renewal. The state was also planning to move all Medicaid determinations, including disability-based determinations, as well as determinations for other social service programs into the new system and to launch a tablet-based application.
The kynect website included features to assist individuals seeking health insurance. These features included informational videos, a countdown clock to the end of open enrollment, an option to subscribe to email updates, a toll-free number, and information about how to obtain local in-person assistance. The website provided resources in other languages as well as a toll-free number for language assistance and a full Spanish version of the website was available. Kynect also launched a mobile app through which individuals could identify enrollment events, find an agent or assister, complete a pre-screen for eligibility, and anonymously shop. It planned to enhance the app over time to allow individuals to create an account, take images of documentation, and browse for plans, including Medicaid managed care plans (Figure 1).
Outreach and Marketing
Kentucky used state-specific branding for kynect, which helped detach the coverage expansions from the ACA or “Obamacare.” This state-specific branding was particularly important in Kentucky, since many residents are distrustful of government programs and not politically supportive of the ACA. Kentucky directed all residents seeking health insurance to “kynect, Kentucky’s Health Care Connection.” It also created animated characters that were representative of different types of Kentuckians who could benefit from the new coverage options, to which stakeholders felt consumers responded well (Figure 2). The effectiveness of the state-specific branding is supported by survey results that show that, although Kentucky residents lean negative in their views of the ACA law as a whole, they are more positive towards the programs the law has created in the state. For example, about half (49%) of residents have an unfavorable view of the health care law, but 42% have a favorable view of kynect and 63% have a favorable view of the Medicaid expansion. However, there remain large gaps in knowledge and understanding of these components of the law, with about 30% saying they don’t know enough to say their view on kynect and 13% not reporting a view on the Medicaid expansion.
I think the approach that the Governor took on this whole thing was to not talk about it in terms of Obamacare or the Affordable Care Act. He talked about it in terms of…Kentucky’s health… it’s not about politics…. It’s about improving the health of our state, so that kind of takes the argument out of it. – kynect official
Kentucky conducted statewide marketing across diverse channels. The state launched an extensive statewide marketing campaign to educate individuals about the new coverage options and used diverse channels, including television, radio, print, billboards, and social media. Messaging during the early part of the initial open enrollment period conveyed a simple, straightforward message about the availability of new coverage options and focused on raising brand awareness of kynect. In year two, outreach messaging shifted away from raising awareness to providing personal testimonials and emphasizing the importance and value of coverage. Stakeholders also indicated that messaging focused more on the availability of financial help and affordable coverage options during year two. For example, kynect’s advertising included the phrase, “If you think you can’t afford to be insured, think again” (Figure 3).
In addition to a broad marketing campaign, the state and other stakeholders engaged in an expansive range of local level enrollment efforts. For example, kynect and Medicaid officials and assisters attended events throughout the state, including the state fair, where they distributed information about coverage options and encouraged people to enroll (see Box 1). They distributed reusable shopping bags at these events, which were viewed as highly effective in raising awareness of kynect. Additionally, kynect officials travelled across the state in branded RVs to promote coverage and get people enrolled. During the initial open enrollment period, kynect also established an enrollment storefront in the community that was staffed with assisters, brokers, and kynect and Medicaid staff. Stakeholders noted that this storefront was enormously successful and particularly helpful for handling complex cases because all of the people with the needed expertise were in the same room. Building on this success, kynect provided two enrollment storefronts during year two as well as enrollment kiosks in various locations. The state and assisters also hosted local enrollment events. For example, kynect promoted a “Sign-up Saturday” event at local libraries. In some cases, assisters used local media outlets to reach large numbers of consumers. For example, some assisters participated in a weekly local news station call-in show, during which consumers could call in with coverage questions.
The state and assisters utilized targeted enrollment efforts to connect with hard-to-reach populations. Stakeholders described focused efforts to reach the Latino community, including utilizing more Spanish-speaking assisters and volunteers and marketing through Spanish media channels. Assisters also targeted outreach to the immigrant community, African Americans, young adults, veterans, and the LGBT community. In addition, the state launched an initiative to enroll individuals in coverage as they re-enter the community upon release from prison or jail.
Box 1: Using the State Fair to Promote Outreach and Branding in Kentucky
The state fair in Kentucky has been a tradition for over 100 years. The fair is held in August at the Kentucky Exposition Center and attracts about 600,000 people annually. The state fair and other festivals and large sporting events across the state served as a key opportunity to provide information about coverage options to large numbers of people. Marketplace and Medicaid officials and assisters hosted informational booths at these events to raise awareness about the coverage options and initiate one-on-one conversations with interested consumers (Figure 4). Officials and assisters found that starting with the question, “Do you know somebody that doesn’t have health insurance?” was a highly effective way to initiate conversations with individuals at these events. In addition, the reusable kynect shopping bags helped engage consumers at these events. These popular, colorful bags included the kynect logo and the caricatures that appeared in ads and other kynect marketing and have been credited with successfully raising awareness of kynect and initiating a marketing buzz. Replicating the logo and characters on t-shirts and even hot air balloons made it difficult to go anywhere in the state without hearing about kynect.
“[The bags] were like gold. I mean they were just really pretty, colorful, and instead of us sitting there talking about healthcare, we’d say, ‘have you heard about kynect, let me tell you about kynect’ and then people would stop and listen, and ‘do you have health insurance,’…and if they said ‘yes, I have health insurance,’ ‘well do you have a child or do you have somebody that you know that doesn’t?’ We made those connections and I think that that was one of our biggest success factors…..” — Medicaid official
Enrollment Assistance
Kentucky established an extensive consumer assistance network that drew on existing assistance networks, including those providing Medicaid and CHIP enrollment assistance, health clinics, community-based organizations, hospitals, and advocacy organizations. Kynectors, as enrollment assisters are called in Kentucky, had varied backgrounds and were able to provide personalized assistance to the communities they served. Some kynectors also said that, because of their personal ties to the community, local organizations, schools, and other groups were often willing to work closely with them and sometimes offered resources, such as space and equipment, to support enrollment. Recruiting trusted members of the community to serve as kynectors was particularly important in rural eastern Kentucky where kynectors achieved significant enrollment success. In addition to kynectors, insurance brokers played an important role in enrollment. Kynect undertook significant efforts to engage brokers in enrollment and, despite some early fears and concerns among brokers, a large number of brokers were certified and often worked collaboratively with assisters to enroll uninsured people. This relationship between kynectors and brokers became increasingly strong over time. Providers, particularly community health centers (CHCs), also played a key role in outreach and enrollment by conducting both in-reach to their uninsured patients as well as outreach to the broader community.
Agents felt very threatened about it, so very early on, both the Commissioner of Insurance and our folks assured agents that they’re going to have a role and they’re going to have a very important role. And so when we set up the advisory board, we established several subcommittees and one of them was a subcommittee called Agents and Navigators. … The idea was that we were going to put the two competing forces … together and see if we couldn’t work out some kind of agreed to relationship. – kynect official
Kentucky utilized a regionally-based hub and spoke structure to organize and coordinate assister activities. Under this model, several lead regional organizations helped organize and coordinate activities of kynectors in their area, disseminated updates and information from the state to kynectors, and provided feedback on implementation to the state. In some areas, broader coalitions of stakeholders also helped coordinate and organize activities. For example, in Louisville, the local Board of Health established an outreach and enrollment coalition that coordinated efforts, shared best practices, and provided feedback on experiences in the field to the state. Kynectors also used shared online calendars to indicate where and when they were planning events, which helped prevent gaps and overlaps in outreach and enrollment efforts.
The state provided readily available support to consumer assisters. Kentucky established resources for kynectors and brokers to obtain support when they had questions or needed assistance while helping a consumer. Kynectors had dedicated telephone lines to reach call center staff, which helped reduce long waits when they needed support. Kentucky also maintained close and regular communication with kynectors to both share updates and information and receive feedback on implementation.
Access to and Utilization of Care
There have been efforts underway at multiple levels to help increase health insurance and health care literacy among individuals. For example, kynect created a “how to kynect” brochure that provides a glossary, information on how to find a primary care provider and how to use care, and healthy living tips. Kynectors have also developed educational materials to help improve health and health care literacy among newly covered individuals.
Medicaid enrollees are accessing needed care. An independent analysis of the first year of the Medicaid expansion in Kentucky found that, compared to previously eligible parents, those in the Medicaid expansion group accessed providers at a higher rate and had increased utilization of preventive services.4 Stakeholders suggest that part of this pattern might be due to the previous lack of health insurance leading to first-time screenings and appointments particularly for diabetes, heart disease, and other chronic conditions. In addition, there has not been a spike in overall emergency room use as had been anticipated.
There are some access challenges for certain types of services and providers. These challenges include access to certain specialties and behavioral health services and access in rural areas. However, stakeholders pointed out that these challenges are reflective of overall provider shortages and not specific to Medicaid. Kentucky engaged in efforts to expand access to behavioral health providers by allowing Medicaid to contract with individual providers (rather than through community mental health centers) and additional provider types (such as licensed drug alcohol counselors) and adding new services to Medicaid (such as additional services for substance use treatment). Stakeholders in Kentucky also pointed to challenges recruiting dental providers, although they noted that access varies across the state, with greater provider availability in Louisville where there is a dental school. As of the end of the second open enrollment period, Kentucky was focused on increasing care management for Medicaid enrollees who are super-utilizers of emergency department care. In addition, Kentucky added behavioral health services into the Medicaid managed care contract in 2014, and was holding regular meetings with the plans and educational forums with behavioral health providers to support integration of these services.
Overall, Kentucky residents, particularly those enrolled in Medicaid, view the program as working well for low-income residents. Among all residents, about two-thirds (67%) feel that the Medicaid program is working well for most low-income people in the state. This share rises to 84% among adults who are actually covered by Medicaid (Figure 5).
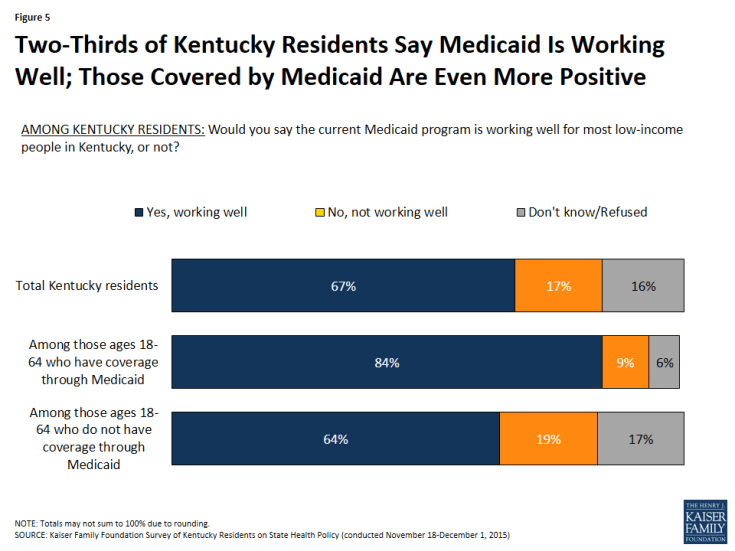
Figure 5: Two-Thirds of Kentucky Residents Say Medicaid Is Working Well; Those Covered by Medicaid Are Even More Positive
Access to care for individuals enrolled in QHPs varies based on their choice of plan. For example, a number of stakeholders noted that some individuals who selected lower cost plans with limited networks experienced challenges getting appointments and finding providers. They suggested that some of these challenges have moderated over time as individuals have adjusted their expectations and some plans have made adjustments to better accommodate member needs.
Economic Impact of Medicaid Expansion
The state has achieved cost savings as a result of the expansion. Overall, estimates show savings resulting from the Medicaid expansion. One analysis estimated a net positive fiscal impact from the Medicaid expansion of $919.1 million from SFY 2014 through SFY 2021 compared to what the state would have spent had it not expanded. These net positive impacts resulted from increased employment, increased revenues to providers, and decreased uncompensated care.5 The analysis also found that the state’s health care system and overall economy realized an infusion of $1.16 billion driven by new federal payments to health care providers for Medicaid expansion enrollees in calendar year 2014.6
What changes are being made to kynect and Medicaid?
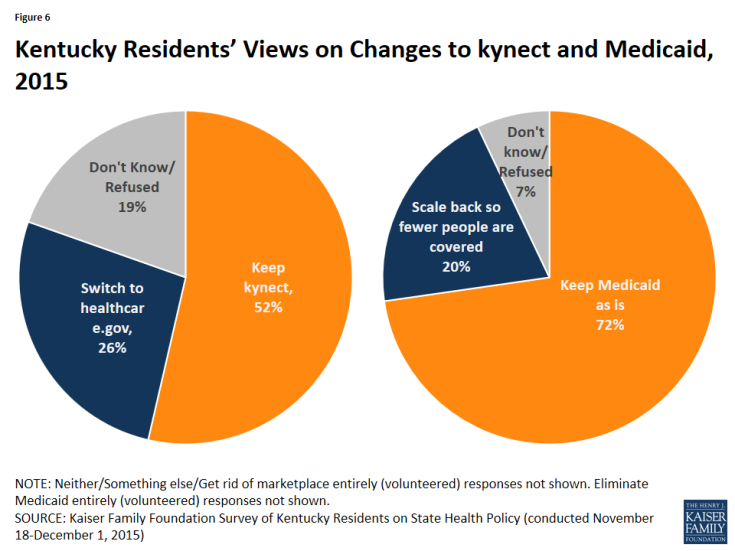
In December 2015, newly elected Governor Bevin took office in Kentucky. Consistent with his election campaign, he has begun making changes to Kentucky’s health coverage system. These changes include transitioning from the fully state-run Marketplace, kynect, to a federally-supported State-Based Marketplace and proposing to make changes to the Medicaid expansion through a waiver.7,8 A Kaiser Family Foundation survey of the views of Kentucky residents completed just after the Governor’s election in 2015 found that about half (52%) of residents would prefer to keep kynect, while roughly a quarter (26%) would prefer to switch to the federal marketplace. Nearly three in four (72%) Kentuckians said they would prefer to keep the state’s Medicaid program as it is rather than scale it back it to cover fewer people (Figure 6).
What are the potential impacts of these changes?
Changes to kynect
When the state transitions to a federally-supported State-Based Marketplace, the federal government will handle all eligibility and enrollment functions for Marketplace coverage through Healthcare.gov. The state will retain responsibility for consumer assistance and will maintain review of plans to include in the Marketplace, but certification of the plans will become a federal government responsibility. Some key questions to consider about the potential effects of this change include the following:
- How will the Medicaid and Marketplace enrollment experience be affected? With this change, there will no longer be an integrated eligibility determination and enrollment system for Medicaid and Marketplace coverage. On February 29, 2016, Kentucky launched Benefind, its new online portal for individuals to apply for Medicaid. Individuals may also apply for the Children’s Health Insurance Program and other programs, including the Supplemental Nutritional Assistance Program (SNAP, formerly food stamps) and Temporary Assistance for Needy Families, through Benefind. The Benefind system now serves as the state’s Medicaid eligibility determination system, while Marketplace determinations will occur through Healthcare.gov beginning in 2017. Once the transition is complete, timely and effective data transfers between Benefind and Healthcare.gov will be key for providing a seamless enrollment experience and preventing delays in eligibility determinations and gaps in coverage. Early experience with Benefind has indicated that system glitches have led to confusion and disruptions in coverage that could compromise enrollment.9
- How will outreach and enrollment assistance be affected? As a federally-supported State-Based Marketplace, the state will retain responsibility for running the navigator (kynector) program. However, funding and other decisions will have important implications for the availability of consumer assistance in the future. For example, the transition to Benefind limited the role kynectors can play in assisting individuals with Medicaid coverage since only state eligibility workers can access the Benefind system.10 In addition, the state ended its advertising campaign that was targeted at raising consumer awareness about coverage options for kynect as of December 2015.11
- How will this transition affect insurer participation and plan offerings in the Marketplace? The state will continue to play a leading role in negotiating with insurers and will make recommendations to the FFM regarding insurer contracts. The state will also continue to regulate the insurers. However, plans will contract with the federal government rather than the state, which may influence their participation decisions. In addition, insurers that were considering entering the market for 2017 may choose to wait out this transition year.
- How much will the transition cost? The specific costs associated with the transition to a federally-supported State-Based Marketplace are uncertain. However, there are costs associated with decommissioning kynect, standing up the new Benefind eligibility system, and building functionalities to connect with Healthcare.gov. At the same time, there are savings related to foregone maintenance and operations costs for kynect and other potential savings that could accrue from reduced funding for consumer assistance and the call center.
From Medicaid Expansion to Waiver
The Governor plans to seek a waiver to make changes to the Medicaid expansion and has noted that he is looking to Indiana’s Medicaid expansion waiver as a potential model. The Governor hopes to have a plan proposed by the middle of 2016 and to implement changes at the start of 2017. To date, six states (AR, IA, MI, IN, NH, and MT) have Section 1115 waivers to implement the ACA Medicaid expansion in ways that extend beyond the law. While the waivers are each unique, they include some common provisions, including use of premium assistance, charging premiums, eliminating coverage of non-emergency medical transportation, and use of healthy behavior incentives.12 Most of the states with approved expansion waivers used the waiver to expand coverage to the uninsured population, resulting in new coverage. Since Kentucky already has its expansion in place, how the waiver affects individuals with existing coverage will be a key consideration. As more details on changes the Governor might seek through a waiver become available, it will be important to consider their impacts on enrollees, providers, costs, and program administration and complexity.
Conclusion
As a leader in implementing the ACA coverage expansions, Kentucky’s experience provides useful lessons about key components that have contributed to its success. These components include strong leadership and collaboration; a high-functioning integrated eligibility system; broad outreach and marketing efforts; a strong and diverse network of enrollment assistance; and initiatives to strengthen access to care for Medicaid enrollees as more individuals enroll. The newly elected Governor is moving forward with changes to transition from the fully state-run Marketplace, kynect, to a federally-supported State-Based Marketplace and plans seek a waiver to make changes to the Medicaid expansion. These changes have the potential to reshape coverage in Kentucky and will be important to track and assess over time.