No Limit: Medicare Part D Enrollees Exposed to High Out-of-Pocket Drug Costs Without a Hard Cap on Spending
Note: A newer version of this analysis with 2017 data is available here.
Since 2006, the Medicare Part D prescription drug benefit has helped improve the affordability of medications for people with Medicare. Yet even with Part D, enrollees can face relatively high out-of-pocket costs because there is no hard cap on out-of-pocket spending under Part D. Enrollees are required to pay up to 5 percent of their drug costs above the catastrophic coverage threshold, unless they receive low-income subsidies that help pay Part D premiums and cost sharing. For high-priced medications, this relatively small coinsurance rate can translate into significant out-of-pocket costs. This analysis examines out-of-pocket prescription drug spending among Medicare Part D enrollees with costs above the catastrophic coverage threshold.
1 million #Medicare #PartD enrollees had high out-of-pocket #prescriptiondrug costs in 2015.
Key Findings
- In 2015, 3.6 million Medicare Part D enrollees had total drug spending above the catastrophic coverage threshold. Of this total, 2.6 million enrollees received low-income subsidies, but 1 million enrollees did not, and incurred out-of-pocket drug spending above the catastrophic threshold.
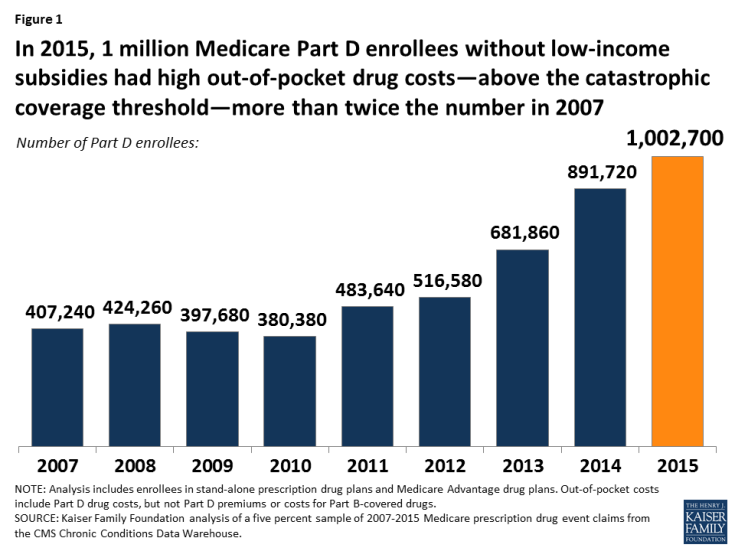
- Between 2007 and 2015, the number of Part D enrollees without low-income subsidies who had spending above the catastrophic threshold more than doubled (Figure 1).
- Part D enrollees with out-of-pocket costs above the catastrophic threshold comprised just 2 percent of all enrollees but 20 percent ($3 billion) of enrollees’ total out-of-pocket drug spending ($15 billion) in 2015.
- The one million Part D enrollees with out-of-pocket costs above the catastrophic threshold spent more than $3,000 out of pocket on their prescriptions in 2015, on average; 1 in 10 of them spent at least $5,200. In total, they spent $1.2 billion out of pocket above the catastrophic threshold, or $1,215 per person.
- Harvoni and Sovaldi, treatments for hepatitis C, topped the list of the 10 most costly drugs used by Part D enrollees with high out-of-pocket drug costs in 2015.
- Among Part D enrollees in stand-alone Medicare drug plans without low-income subsidies, those with HIV/AIDS, multiple sclerosis, viral hepatitis, leukemia/lymphoma, and schizophrenia were more likely than those with other conditions to have out-of-pocket spending above the catastrophic threshold in 2015.
- Average out-of-pocket costs by Part D enrollees with spending above the catastrophic threshold declined substantially between 2010 and 2011, due to the Affordable Care Act provisions that took effect in 2011 to close the coverage gap and provide a 50 percent manufacturer discount for brand drugs, the value of which counts as out-of-pocket spending. Since 2013, however, average out-of-pocket spending among this group has increased due in part to the growing availability and use of high-priced drugs.