The independent source for health policy research, polling, and news.
Continuous Eligibility Policies Can Reduce the Number of Children Who Lose Medicaid Despite Still Being Eligible for Coverage
A new KFF analysis finds disenrollment rates were lower in the 12 months leading up to annual renewals for children in states with 12-month continuous eligibility compared with states without the policy. Congress is expected to pass an omnibus spending bill by the end of the year that would require 12-month continuous eligibility for children in all states.
The analysis also finds that in states with 12-month continuous eligibility, a smaller share of children disenrolled from Medicaid and then re-enrolled within the year – a phenomenon known as “churn.” Churn often indicates children are losing coverage due to administrative burdens even if they remain eligible for coverage.
In the study, KFF analysts used Medicaid claims data to measure enrollment outcomes among a cohort of children newly enrolled in Medicaid in July 2017 in states with and without 12-month continuous eligibility.
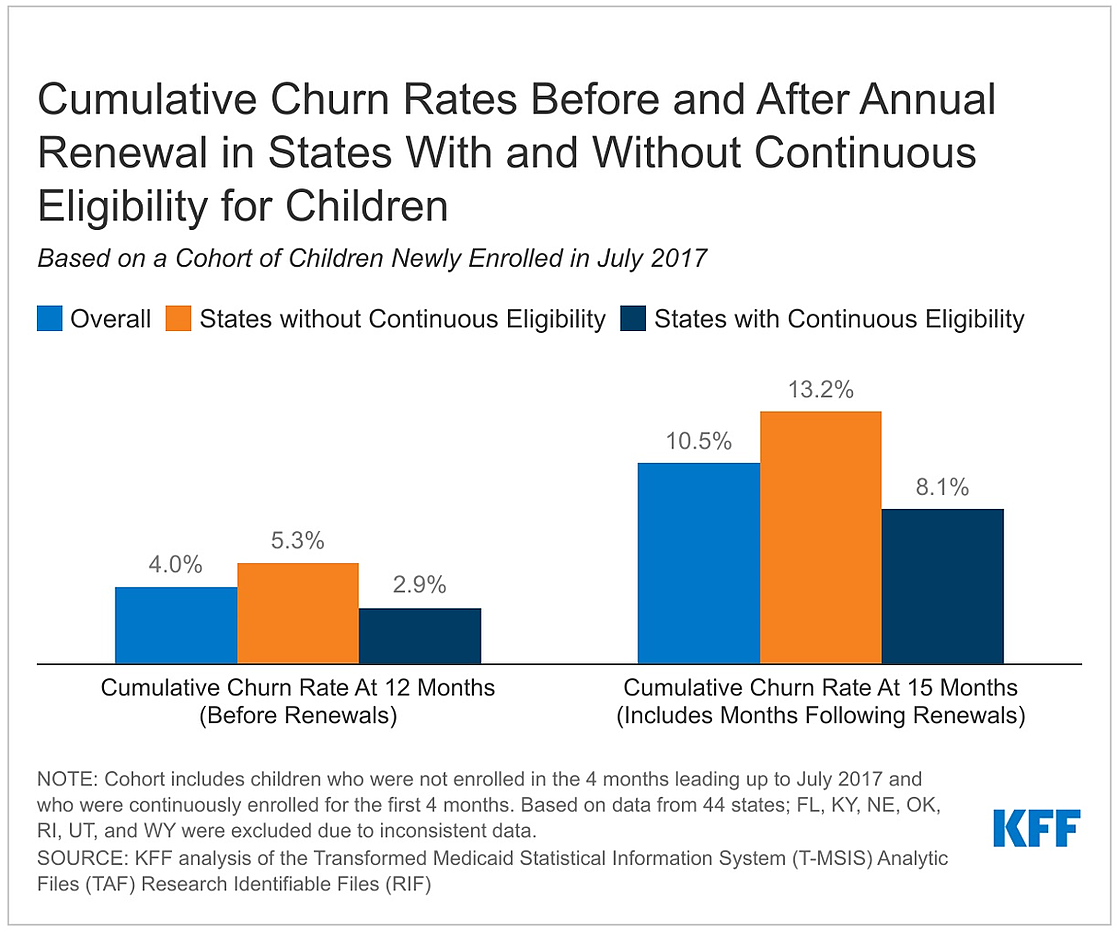
By month 12 (before annual renewals), the share of children who “churned” was 2.9% in states with 12-month continuous eligibility policies and 5.3% in states without continuous eligibility.
The analysis also shows that following annual renewals, the cumulative disenrollment rate more than doubled, some of which is to be expected with family income changes. However, churn also increased – from 4.0% in month 12 to 10.5% in month 15, signaling many eligible children are losing coverage at their annual renewal. Churn and disenrollment rates increased sharply in states with and without 12-month continuous eligibility following annual renewal, though increases were larger in states without 12-month continuous eligibility.
While churn rates increased among all racial/ethnic groups following annual renewal, the increase was largest for Hispanic children, growing from 5.2% in month 12 to 12.5% in month 15.
These finding have implications for the end of the federal continuous enrollment requirement, when all states will be required to conduct renewals for all individuals on Medicaid. Millions of people, including children, could lose coverage if they are no longer eligible or face administrative barriers during the process despite remaining eligible. The omnibus spending bill would end the continuous enrollment requirement as of March 31, 2023 and phase out the enhanced match rate through the end of 2023.
About 37.8 million children were enrolled in Medicaid as of August 2022, with about half of those children in states with 12-month continuously eligibility and about half in states without the policy. Expanding 12-month continuous eligibility to all states likely would reduce the number of children who are uninsured but would come at a price of higher federal and state Medicaid spending.
The findings also suggest that multi-year continuous eligibility policies could help children maintain coverage beyond one year. To extend continuous eligibility for children for multiple years or for adults for 12 months or longer, states must use the Section 1115 waiver process and obtain approval from the Centers for Medicare and Medicaid Services (CMS).
Oregon was the first state to get CMS approval for such a waiver. It will provide continuous eligibility for children in Medicaid from birth until age six as well as two years of continuous eligibility for all enrollees ages six and older. Other states, including California, New Mexico, and Washington state, have proposals in development or pending approval from CMS.