Medicaid Coverage of Pregnancy and Perinatal Benefits: Results from a State Survey
Correction: While KY and MS responded to the survey that their states cover doula services, subsequent research has found that the states do not cover doula services. To our knowledge, OR and MN, and as of January 2021, NJ, are the only states currently covering doula services.
Prenatal Services
Prenatal care services monitor the progress of a pregnancy and identify and address potential problems before they become serious for either the mother or baby. Increasing the share of pregnant women who begin care in the first trimester is one of the national objectives of the federal government’s Healthy People 2020 initiative.1 Routine prenatal care encompasses a variety of services, including provider counseling, assessment of fetal development, screening for genetic anomalies, prenatal vitamins that contain folic acid and other nutrients, and ultrasounds, which provide important information about the progress of the pregnancy.
PRENATAL VITAMINS AND ULTRASOUND
| Key Finding: Prenatal Vitamins and Ultrasound |
| All states cover prenatal vitamins and ultrasounds for pregnant women. Some states impose quantity limits or require a prescription for vitamins. |
All states that responded to the survey reported that they cover prenatal vitamins and ultrasounds for pregnant women regardless of eligibility pathway (Table 4). Some states impose limitations on this coverage however, such as requiring a prescription for prenatal vitamins or limits on the number of ultrasounds allowed during the course of a pregnancy.
| Table 4: Coverage and Utilization Controls for Prenatal Vitamins and Ultrasounds | ||||
| Traditional Medicaid (n=41) |
Medicaid ACA Expansion (n=25) |
Pregnancy Only Medicaid (n=41) |
||
| Prenatal Vitamins | 41 | 25 | 41 | |
| Ultrasound | 41 | 25 | 41 | |
| Limitations and Utilization Controls | ||||
| Prenatal Vitamins | Ultrasound | |||
| Prescription or other documentation (4) | AK, CO, CT, NY | |||
| Price/quantity controls (6) | AR | AL, CO, MO, SC, TX | ||
| Prior Authorization to exceed state quantity limits (3) | AL, SC, TX | |||
| Age limitations (1) | MS – limited to ages 8-50 | |||
| Preferred Drug List (PDL) (1) | MS | |||
| Pregnancy status (e.g. high-risk) (2) | TX, WV | |||
Appendix Table A1 provides state detail for states’ prenatal service coverage policies.
Genetic Screening Services
| Key Finding: Genetic Screening Services |
| Nearly all responding states reported covering CVS and amniocentesis across all eligibility pathways available in the state, but fewer states reported covering genetic counseling service, which is generally limited to women with higher risk or for those that have a positive result in genetic screens. |
| Table 5: State Coverage for Genetic Lab and Counseling Services | ||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy Only (n=41) |
Not Covered in Any Pathway (n=41) |
|
| Genetic Counseling | 33 | 21 | 33 | 8 |
| Chronic Villus Sampling | 38 | 24 | 38 | 3 |
| Amniocentesis | 39 | 24 | 39 | 2 |
Routine prenatal care typically includes ultrasound and blood marker analysis to determine the risk of certain birth defects such as sickle cell, down syndrome, or other birth abnormalities. While these tests are effective screening tools to determine risk, they are not diagnostic. If the results of screening tests are abnormal, genetic counseling is recommended and additional testing such as chorionic villus sampling (CVS) or amniocentesis may be needed.
States were questioned about their policies with respect to genetic counseling, CVS, and amniocentesis testing for pregnant women. Of the 41 responding states, 33 reported covering all three services across all eligibility pathways (Table 5). Genetic counseling is covered in fewer states than either of the screening tests. The eight states that do not provide genetic counseling services through any Medicaid pathway are Alabama, Alaska, Arizona, Idaho, Nebraska, New Mexico, West Virginia, and Wyoming. Only one state, Nebraska, does not cover any of the three services under any of its eligibility pathways, but the state noted that genetic testing is covered for the mother and baby with prior authorization after delivery. Few states reported utilization controls or limitations. Medical necessity and an indication of risk for genetic anomalies were the most frequently noted restrictions. Appendix Table A2 provides detail on state Medicaid policies for genetic testing and counseling.
Counseling and Support Services
There are a variety of support services that can aid pregnant and postpartum women with pregnancy, delivery, and child rearing. These include educational classes on childbirth and infant care, transportation to appointments, and home visits during or after pregnancy to assist with basic medical care, counseling on healthy behaviors, and in person infant care assistance.
Childbirth and Parenting Education
| Key Finding: Childbirth & Parenting Education |
| Less than half of the responding states report that they provide education services to support childbirth, infant care or parenting in any of the Medicaid eligibility pathways. |
Less than half of responding states reported that they cover childbirth and parenting education for pregnant women (Table 6). The 13 states that cover both services are: Arkansas, California, District of Columbia, Delaware, Georgia, Hawaii, Michigan, Minnesota, Mississippi, Ohio, Oregon, Virginia and Washington. Conversely, two-thirds of states indicated they do not cover childbirth education in any of their programs (27 of 41 states) and over half indicated they do not cover formal or standalone infant care or parenting education (24 of 41 states). Among the states that reported that they do not cover educational services, some stated that such services are available through other public programs and some reported they provide education as part of prenatal visits. See Appendix Table A3 for details on states’ coverage of childbirth and parenting education.
| Table 6: State Coverage for Childbirth and Parenting Education Services | ||||
| Traditional Medicaid (n=41) |
Medicaid ACA Expansion (n=25) |
Pregnancy Only Medicaid (n=41) |
Not Covered in Any Medicaid Program |
|
| Childbirth Education | 14 | 9 | 14 | 27 |
| Infant care/Parenting education | 17 | 12 | 17 | 24 |
Case Management and Substance Abuse Treatment
| Key Finding: Case Management and Substance Abuse Services |
| Over three quarters of responding states indicated that they cover case management services for pregnant women across all Medicaid eligibility pathways. Nearly all states surveyed reported that they cover substance/alcohol abuse treatment for pregnant women |
Case management can help pregnant women obtain and coordinate services that may be available from multiple providers. Six states do not provide case management in any Medicaid pathway: Connecticut, Hawaii, Maryland, Michigan, New Hampshire, and South Carolina. While the service is not separately billable, Connecticut notes that case management would be covered as part of a hospital admission or through a clinic or office visit. Most of the remaining 35 states provide case management through all eligibility pathways, with exceptions noted in Appendix Table A4.
Case management is often limited to women at higher health risk, or with medical conditions. For instance, Missouri noted that participants must qualify for case management services; Nebraska does not provide the benefit universally, rather it is based on the need of the individual; West Virginia provides the service through its targeted case management program based on medical need. Four states also noted that the case management benefit is provided through managed care or utilization management contracts.
Misuse of alcohol and other substances during pregnancy is correlated with a wide range of negative infant outcomes, including premature birth, fetal alcohol syndrome, and infant drug withdrawal. The ACA requires states to cover counseling services for alcohol misuse for beneficiaries enrolled under the ACA’s Medicaid expansion option.
All states surveyed reported that they cover substance/alcohol abuse treatment for pregnant women in at least one Medicaid eligibility pathway and most states align coverage across pathways (Table 7). New Hampshire is the only state that reported it does not cover substance abuse treatment in its traditional Medicaid pathway. Appendix Table A4 provides detail around state coverage of case management services and substance and alcohol use treatment for pregnant women.
| Table 7: Number of States Covering Counseling and Support Services | |||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy Only (n=41) |
Not Covered in Any Program (n=41) |
Utilization Controls | |
| Case Management | 35 | 19 | 32 | 6 |
|
| Substance/ Alcohol Abuse Treatment | 40 | Required | 38 | ||
Home Visiting Services
| Key Finding: Home Visiting Services |
| Most of the responding states indicated they cover prenatal and postpartum home visits. |
Home visits both during and after pregnancy can help pregnant and postpartum women care for themselves as well as their newborns. Typically conducted by nurses and social workers, they may use the time at home visits to counsel new and expectant parents on a wide range of subjects related to healthy pregnancies and raising healthy children, such as diet and nutrition, basic infant care, breastfeeding, and positive child development. These visits are meant to provide the time for deeper, one-on-one contact and counseling that pregnant women and new parents may not have during routine prenatal and well-baby appointments. Research has found that home visits are associated with a variety of positive outcomes, including lower severity of postpartum depression and improved mother-child interactions.2 Home visits may also cover management of substance abuse, depression, and other chronic conditions. As shown in Table 8, over a quarter of responding states do not provide prenatal home visit supports in any Medicaid program (11 of 41 states). Nearly one fifth (8 of 41 states) do not provide postpartum home visit supports. Of the 30 states that cover both prenatal and postpartum home visits, nearly all provide the service across all eligibility pathways.
Three states provide postpartum home visits but do not provide prenatal home visits through any pathway: Alabama, Maryland and Tennessee. Some states cover prenatal or postpartum home visits under limited circumstances. For example, Michigan notes that the state allows three postpartum home visits only when a physician has determined the mother or newborn to be at risk. Appendix Table A5 details state coverage policies on home visiting services.
| Table 8: Number of States Covering Prenatal and Postpartum Home Visits | |||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy Only (n=41) |
Not Covered in Any Program (n=41) |
Utilization Controls | |
| Home Visit- Prenatal | 30 | 17 | 29 | 11 |
|
| Home Visit- Postpartum | 33 | 19 | 31 | 8 |
|
Delivery and Postpartum Care
| Key Finding: Delivery & Postpartum Care |
| A majority of responding states reported that they cover deliveries in birth centers but only half cover home deliveries. Very few states noted utilization controls for delivery options, and usually restrictions are related to provider requirements. Four states reported covering doula assistance. |
The survey questioned states about the provision of specific delivery services including deliveries at birth centers, home births, doula assistance, and postpartum visits. A doula is a trained non-clinician who assists a woman before, during and/or after childbirth, by providing physical assistance, labor coaching, emotional support, and postpartum care.
Birth center delivery is more likely to be a covered benefit than is home birthing (Table 9). Over three-quarters of responding states (32 of 41) cover deliveries in birth centers compared with about half (21 of 41) covering home births. All states that cover the options within their traditional Medicaid program also provide coverage across all eligibility pathways available within the state. Per the ACA, coverage for deliveries at birth centers is required in all states that license such facilities. There is no comparable requirement for coverage of home births, but in states that have chosen to cover home births, some such as Colorado and Virginia reported that the births must be performed by Certified Nurse Midwives.
All states covered postpartum visits in all eligibility pathways except Oklahoma which does not cover the benefit in its program for pregnant women. Illinois and Texas allow reimbursement for one postpartum procedure per pregnancy. In Texas, the reimbursement covers all postpartum care regardless of the number of visits provided.
Conversely, the only states that cover doula services are Kentucky, Minnesota, Mississippi and Oregon, and they cover the service in all available eligibility pathways.3 Appendix Table A6 presents state coverage of delivery options and postpartum care.
| Table 9: States Covering Delivery Services | ||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy Only Medicaid (n=41) |
Not Covered in Any Program | |
| Birth Centers | 32 | 21 | 32 | 9 |
| Home Births | 21 | 15 | 21 | 20 |
| Doula Services | 4 | 3 | 4 | 37 |
| Postpartum Visit | 41 | 25 | 40 | 0 |
Breastfeeding Services
Raising breastfeeding rates is one of the country’s national Healthy People 2020 goals.4 There is a range of supports that have been found to help women initiate and maintain breastfeeding, including breast pumps, lactation counseling by certified consultants both inpatient and outpatient after delivery, and educational programs, which can begin during pregnancy and continue after the birth of a child. States are required to cover breast pumps and consultation services for Medicaid expansion beneficiaries under the ACA’s preventive services requirement.
Breast Pumps
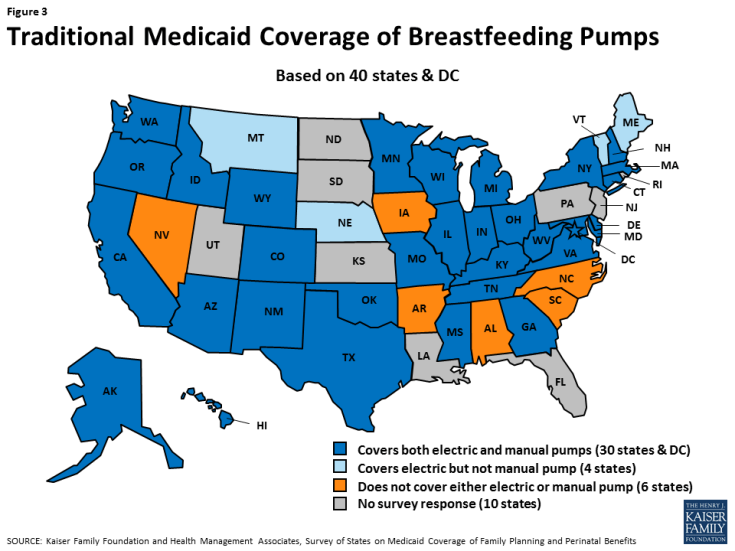
| Key Finding: Breast Pump Coverage |
| A majority of responding states cover both electric and manual breast pumps, but some report using various utilization controls such as prior authorization or quantity limits. |
Most responding states report that they cover electric breast pumps (35 of 41 states) and manual pumps (31 of 41 states) in their traditional Medicaid program (Table 10).5 All states that cover pumps in their traditional Medicaid program also cover the benefit in all eligibility pathways except Illinois and Oklahoma, which do not provide the benefit in their program for pregnant women. Six states do not provide either electric or manual pumps under either their traditional Medicaid program or their pregnancy-only eligibility pathway: Alabama, Arkansas, Iowa, North Carolina, Nevada, and South Carolina (Figure 3).6
| Table 10: Breastfeeding Supplies | |||
| Traditional Medicaid (n=41) |
Pregnancy Only Medicaid (n=41) |
Not Covered in Any Pathway (n=41) |
|
| Electric Breast Pump | 35 | 33 | 6 |
| Manual Breast Pump | 31 | 29 | 10 |
| *While coverage of breast pumps is required for all ACA Medicaid expansion enrollees, coverage detail regarding the type of pump covered was not reported by Arkansas, Iowa or Nevada. | |||
Breast Pump Utilization Controls
Several states reported utilization controls for breast pumps. As shown in Table 11, prior authorization is the most frequently employed utilization control, followed by quantity/time limits. Some states noted multiple utilization policies. For instance, Colorado requires prior authorization for electric pumps. The state allows rental or purchase of a breast pump based on the situation of the infant or mother. The state covers rental of an electric pump when the infant is expected to be hospitalized for less than 54 days, but allows breast pump purchase for hospital stays expected to last longer than this.
For quantity/time limits, Massachusetts limits the purchase of either an electric pump or manual to one per member every five years. Ohio limits electric pumps to one every five years, and a manual pump to one every 24 months but did not specify rental or purchase requirements. Texas limits the purchase of an electric or manual breast pump to one every three years, but does not time-limit the rental of a hospital grade pump. Appendix Table A7 provides policy detail around state Medicaid coverage for breast pumps.
| Table 11: Utilization Controls Applied to Breast Pump Benefit | |
| Utilization Control | States with Utilization Policy |
| Prior Authorization (7) | CO, MA*, MI*, MO, MT, OH*, WA |
| Limited to mothers with critical care/NICU infants (3) | CO, MI, TN |
| Quantity/time limits (4) | MA, MI, OH, TX, |
| Conditions determine rental or purchase (3) | CO, MI, TX* |
| Limited to rental (2) | Rental: MT, WA |
| *MI: Prior authorization is not required when standards of care are met. It is required for rental beyond 3 months. MA and OH: Prior authorization required to exceed quantity limit. TX: Purchase of a breast pump is limited to one per three years. Rental is not time-limited. |
|
Breastfeeding Education and Lactation Consultation
| Key Finding: Breastfeeding Education and Lactation Consultation |
| Most responding states reported that breastfeeding education and hospital-based lactation consulting services are covered under traditional Medicaid, but most states do not provide lactation consultation in settings other than a hospital. |
The survey asked about coverage for breastfeeding education such as classes and about coverage for lactation consultation in the hospital, clinic/outpatient, and home settings. There is more variation across the states in the coverage of breastfeeding education and consultation than for breast pumps. As shown in Table 12, 27 of 41 responding states cover breastfeeding education under traditional Medicaid. Individual lactation consultant services are most likely to be covered in the hospital setting. Nearly two-thirds of states responding to the survey stated they cover services in the hospital compared with a little over one-third of responding states providing the service in an outpatient/clinic setting, and less than a quarter of states providing the benefit for postpartum women in their homes.
States did not report utilization controls for breastfeeding support services but a few states noted provider requirements. For example, Connecticut allows the services in hospital and clinic settings if provided by any of these licensed provider types: Physician, DO, Physician Assistant, Advanced Practice Registered Nurse (APRN), or Certified Nurse Midwife (CNM), and is a component of the hospital or clinic reimbursed services. In New York, qualified practitioners for Medicaid reimbursable lactation counseling must be state licensed, registered, or certified health care professionals who are International Board Certified Lactation Consultants (IBCLCs) credentialed by the International Board of Lactation Consultant Examiners (IBLCE) and one of the following: Physician, Nurse Practitioner, Midwife, Physician Assistant, Registered Nurse.
| Table 12: State Coverage for Breastfeeding Support Services | ||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy-Only Medicaid (n=41) |
Not Covered in Any Program (n=41) |
|
| Breastfeeding Education | 27 | 15 | 26 | 14 |
| Individual Lactation Consultation | ||||
|
26 | 16 | 25 | 15 |
|
16 | 12 | 15 | 25 |
|
11 | 10 | 11 | 30 |
Alignment Across Eligibility Pathways and Reimbursement Mechanisms
In the 27 states that cover breastfeeding education in their traditional Medicaid program, coverage is aligned across the three Medicaid eligibility pathways, except in Nevada, which provides the service under traditional Medicaid, but not through the ACA Medicaid expansion or through the state’s program for pregnant women.
However, there is more variation between eligibility pathways for coverage of lactation consultation. Of the 26 states that cover individual lactation services, only 11 cover hospital-based, outpatient, and home consultations services in all of the eligibility pathways available in the state: Arkansas, California, Connecticut, District of Columbia, Delaware, Hawaii, Minnesota, Mississippi, New York, Ohio, and Oregon. All of the 26 states cover inpatient consultation in all of their pathways, with the exception of Oklahoma in the pregnancy only pathway.
Many states reported that reimbursement for lactation consultation is not a separately reimbursable service but is included as a component of other services provided (Table 13), most frequently as a component of hospital reimbursement (11 states). For example, Connecticut noted that the service is not a separately billable service but it is covered as part of a clinic/office visit or hospital stay.
| Table 13: Reimbursement Methodologies for Lactation Consultant Services | ||
| Included in Hospital DRG or Global Fee (10) | Included in Outpatient Clinic Visit (3) | Included in Home Visit (2) |
|
|
|
| * Colorado provides the service as a part of problem specific care, or a special program service such as the Nurse Home Visitor Program but not separately reimbursable. | ||
Appendix Table A8 reports coverage policies for breastfeeding education services across the states. Appendix Table A9 presents information on states’ coverage of lactation consultation and Appendix Table A10 compares coverage within states between eligibility pathways.