Medicaid Coverage of Family Planning Benefits: Results from a State Survey
Introduction
Overview
Medicaid is the primary funding source for family planning services for low-income women. While the federal and state governments jointly finance the program, states operate their programs and establish benefits, eligibility and coverage policies subject to broad federal guidelines. To understand variations in the scope of coverage for family planning and perinatal services and related state Medicaid policies across the nation, the staff of the Kaiser Family Foundation and Health Management Associates surveyed states about benefit policies in place as of July 1, 2015, for family planning and perinatal services.
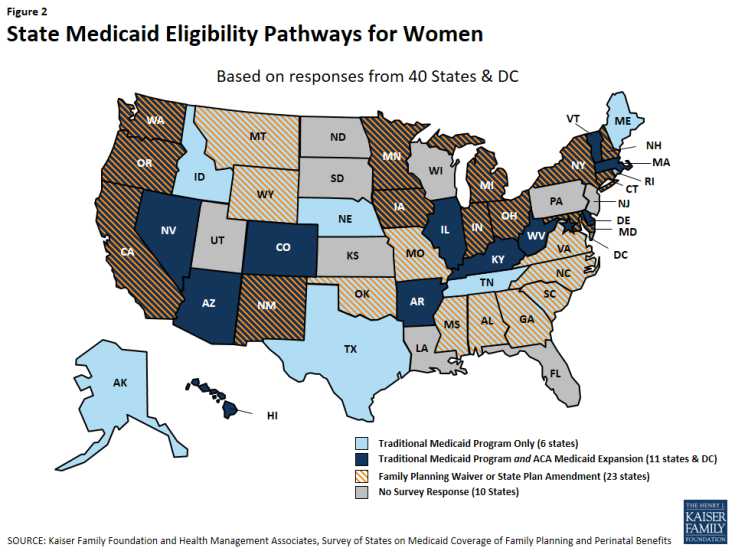
The survey was conducted between October 2015 and February 2016. Forty states and the District of Columbia responded to the survey. Non-responding states are: Florida, Kansas, Louisiana, New Jersey, North Dakota, Pennsylvania, Rhode Island, South Dakota, Utah and Wisconsin. A majority of the states responding to the survey contract with managed care organizations (MCOs) under a capitated structure to deliver Medicaid services, including family planning. While the survey asked states to consider only state Medicaid policies under fee-for-service when responding to the questions, it is possible that MCOs provide additional family planning services to enrollees as added value benefits, unless they are contractually prohibited from doing so.
As illustrated in Figure 2, of the 41 responding states, as of July 1, 2015:
- 25 had adopted an ACA Medicaid expansion program 1
- 23 had a family planning-only waiver or SPA2
- 13 had both an ACA expansion program and a family planning-only waiver or SPA program
- 6 provide services through their traditional Medicaid program only, although one (Texas) also has an exclusively state-funded family planning program.
This report presents the survey findings on 41 states’ Medicaid coverage of family planning services as of July 2015 (DC is referred to as a state throughout this report, for simplicity). Summary tables are presented throughout the report and more detailed, state-level tables are in Appendix A. A companion report summarizing state Medicaid coverage of perinatal services will be issued in the near future.
Background
The manner in which family planning services are financed and organized is unique within the Medicaid program. Federal law:
- Classifies family planning services and supplies as a “mandatory” benefit category that states must cover, but states have some discretion as to which services they include in this category;
- Prohibits copayments or any other form of patient cost sharing for family planning services;
- Entitles beneficiaries to seek family planning services from any provider that participates in the Medicaid program, called freedom of choice; and
- Provides a 90% federal matching rate for the costs of family planning services, a higher proportion than for other services. States pay the remaining 10% of costs.
In addition to long-standing coverage under traditional Medicaid programs, states have also applied to the federal government via “Section 1115 Medicaid waivers” establish programs that extend Medicaid coverage for family planning services only to women and men who are not otherwise eligible for full-scope Medicaid. Prior to the ACA, waivers were the only mechanism for states to establish these limited scope programs. The waivers must be approved by the Centers for Medicare and Medicaid Services (CMS), the federal agency that oversees the Medicaid program. Multiple studies have found that these programs prevent unintended pregnancies and abortions, thus improving women’s health and saving money for the federal and state governments.3
The ACA made many changes to Medicaid coverage that affected beneficiaries’ access to family planning services under the program. Beginning in 2014, states could expand Medicaid eligibility to most people with incomes below 138% FPL without regard to categorical eligibility. As of March 14, 2016, 31 states and the District of Columbia have chosen to adopt full scope Medicaid expansion programs.4 ACA also defined a minimum “Alternative Benefit Plan” (ABP) that states must provide to beneficiaries under this full scope Medicaid expansion option. The ACA specifies that the ABP must include ten “essential health benefits,” including preventive services, at no cost to the patient.5 The preventive services under this policy include several services related to family planning, such as all FDA-approved contraceptives with a prescription, testing for sexually transmitted infections, screening for cervical and breast cancers, the HPV vaccine, and screening for intimate partner violence. Traditional, pre-ACA Medicaid programs and waiver-specific programs, however, are not bound by the ABP requirements, which means that the benefits package can vary within states for different Medicaid populations based on their eligibility pathway (Appendix B).
The ACA also eased the process for states to establish limited scope family planning programs, enabling them to change their program by adopting “state plan amendments,” or SPAs, without requesting a federal waiver of Medicaid rules. States could continue to operate their family planning programs under the waivers as they had historically done, or they could establish the program under SPA authority.
| Table 2: Medicaid Eligibility Pathways for Family Planning Services |
| Traditional Medicaid – Medicaid coverage available prior to the Affordable Care Act (ACA) was based on an individual having income below states’ very low thresholds as well as being in one of the program’s eligibility categories: pregnant, mothers of children 18 and younger, disabled, or over age 65 |
| ACA Medicaid Expansion – The ACA allowed states to eliminate categorical requirements and extend Medicaid to most women and men with family income at or below 138 percent of the federal poverty level. |
| Family planning-only programs – Several states operate programs that provide Medicaid coverage just for family planning services to women who are not otherwise eligible for full Medicaid benefits. These programs are authorized either with waivers or State Plan Amendments (SPAs) that must be approved by CMS. |
There is a minimum floor of family planning services that must be covered under ACA Medicaid expansion, but that is not the case for traditional Medicaid or family planning-only coverage (Table 2). This survey asked states about the scope of states’ coverage of family planning benefits under multiple eligibility pathways for Medicaid. Detailed findings from 40 states and DC on commonalities and differences between and within states are presented for reversible contraceptives, sterilization services, fertility diagnosis and treatment, related sexual health services such as cancer treatment and partner violence screening, and managed care policies.