Medicaid Enrollment Under the Affordable Care Act: Understanding the Numbers
As increasing data become available on the number of people enrolled in coverage under the Affordable Care Act (ACA), there has been interest in the number that have gained coverage through Medicaid and the role of the ACA in these Medicaid coverage gains. The ACA is anticipated to lead to significant gains in Medicaid enrollment as a result of two key changes:
- An expansion in Medicaid eligibility to nearly all adults with incomes at or below 138% of the federal poverty level effective January 1, 2014. While this expansion was intended to occur nationwide, the Supreme Court ruling on the ACA effectively made it a state option, and 26 states are implementing the expansion in 2014.1
- New streamlined Medicaid eligibility and enrollment policies and a single application for Medicaid, CHIP, and subsidized Marketplace coverage. All states must implement these simplifications, which are designed to better connect eligible people to coverage, regardless of whether they implement the expansion.
According to the Congressional Budget Office, by 2016, the ACA is expected to reduce the number of uninsured by 25 million, with a 12 million increase in Medicaid enrollment.2 Overall, an estimated 29% of the current 47.6 million uninsured are eligible for Medicaid in their state.3
How many People have applied for Medicaid since open enrollment began for the new health insurance marketplaces?
CMS reports that state Medicaid and CHIP agencies received a total of 6.6 million applications between October and December 2013.4 This number does not reflect the total number of individuals applying since an application may include more than one person. Moreover, the total number of applications submitted for Medicaid and CHIP over this period is likely higher because this number does not reflect Medicaid and CHIP applications that have been submitted through the State Based Marketplaces (SBMs) and the Federally Facilitated Marketplace (FFM), where many individuals have been directed to apply since open enrollment began in October.
It is difficult to draw conclusions about changes in application volume by comparing changes in new applications to Medicaid and CHIP agencies to baseline data. Because individuals are now applying through multiple pathways, comparisons of application volume to Medicaid and CHIP agencies before and after the ACA will not reflect Medicaid and CHIP application activity now occurring through the Marketplaces. For example, comparisons of application volume to Medicaid and CHIP agencies before and after the beginning of open enrollment show declines in some states, but this may be attributable to a shift in applications from Medicaid and CHIP agencies to SBM or FFM enrollment pathways. Overall, between October and December 2013, CMS reports that over 1.8 million applications for Medicaid, CHIP, or premium tax credits for Marketplace coverage were submitted to SBMs.5 In addition, separate data from HHS show that over 2.7 million applications for Medicaid, CHIP, or Marketplace coverage were submitted through the FFM. It is not possible to disaggregate what share of these applications was for Medicaid or CHIP.6
How many people have enrolled in Medicaid since open enrollment began for the new Health Insurance Marketplaces?
CMS data show that, between October 1, 2013 and December, 31 2013, state Medicaid and CHIP agencies and the SBMs made over 6.3 million total new eligibility determinations for Medicaid and CHIP.7 These reflect determinations for all Medicaid eligibility groups, not just adults made newly eligible for Medicaid by the expansion. However, the data do not reflect Medicaid and CHIP assessments and determinations through the FFM, which is operating in 36 states. In separate data, HHS reported that, as of the end of December 2013, the FFM and SBMs had determined or assessed nearly 1.6 million individuals as eligible for Medicaid or CHIP, with nearly half (751,000) performed by the FFM.8 The Marketplace data aggregates Medicaid and CHIP determinations and assessments and is not directly comparable to the CMS determination data. For “assessment states” the FFM will transfer the accounts to the state to make a final determination of Medicaid eligibility.
What is the role of the ACA in recent Medicaid coverage gains?
The ACA is expected to increase coverage among adults made newly eligible by the Medicaid expansion as well as among already eligible individuals who were not yet enrolled. In states implementing the Medicaid expansion, millions of low-income adults became newly eligible for the program as of January 2014. Moreover, in all states, more people who were already eligible for the program, including children, are enrolling as they are connected to coverage through broad outreach efforts and the new simplified enrollment processes that all states must implement. Past experience with the implementation of the Children’s Health Insurance Program (CHIP) similarly shows that increases in both CHIP and Medicaid enrollment helped significantly reduce the number of uninsured children through the combined effects of eligibility expansions, simplified enrollment processes, and broad outreach and enrollment efforts.9
The new Medicaid enrollment data do not provide for a separate breakout of the number of enrollees who were made newly eligible by the Medicaid expansion, and it is difficult to quantify the impact of outreach and the new streamlined enrollment processes on enrollment. Moreover, because states are in varied stages of readiness to report the eligibility and enrollment data, there are gaps and limitations in the data that constrain analysis of the early data.10 However, broad comparisons to previous Medicaid enrollment trends suggest that the ACA is having a positive impact on Medicaid enrollment.
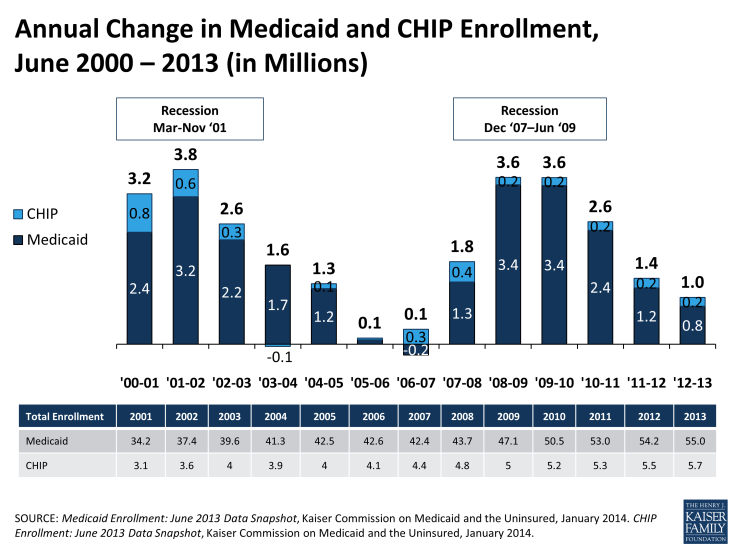
Enrollment trends prior to open enrollment show Medicaid enrollment growth peaking during the recession and then slowing as the economy started to recover. Medicaid enrollment is driven by both changes in economic conditions and policy changes. During the recent economic downturn, as unemployment rates climbed and incomes fell, more people became eligible and enrolled in Medicaid. This increased demand, combined with the maintenance of effort (MOE) provisions that helped preserve coverage (which were first enacted as part of the American Recovery and Reinvestment Act and then maintained under the ACA) led to substantial net annual growth. At the height of the economic downturn, monthly Medicaid and CHIP enrollment grew by 3.6 million between June 2008 to 2009 and June 2009 to 2010.11 Since then, economic conditions have continued to slowly improve, resulting in slower enrollment growth, far below recessionary peaks, at 1.4 million between June 2011 and 2012 and 1.0 million between June 2012 and 2013 (Figure 1).12 These changes reflect a net change in individuals coming on and leaving the Medicaid program.
The 6.3 million Medicaid and CHIP eligibility determinations reported by CMS since the beginning of open enrollment outpaces previous Medicaid enrollment trends. While the CMS reported 6.3 million Medicaid and CHIP determinations made since the start of open enrollment is not directly comparable to monthly Medicaid enrollment data, the volume of determinations made exceeds net Medicaid enrollment gains at the height of the Great Recession and also significantly exceeds the net change in monthly enrollment between June 2012 and June 2013 when economic conditions improved. Overall, total Medicaid enrollment gains since open enrollment began could be higher than the reported 6.3 million determinations because they do not include Medicaid and CHIP assessments and determinations processed by the FFM and because some states did not report CHIP enrollment data; however, the number of new determinations could be lower because some states included renewals in this count, although it is not possible to identify the share that are renewals. In addition, these data may be revised by CMS as it continues to work with states to improve the data collection and reporting.
Looking ahead, future CMS data releases are anticipated to show continued Medicaid coverage gains through the end of the open enrollment period for the Marketplaces and beyond. Enrollment in Medicaid is not limited to open enrollment periods, so individuals may continue to enroll over the course of the year. CMS plans to enhance and expand the data it reports on Medicaid eligibility determinations and enrollment. As the data improve, it will allow for greater analysis both within and across states and of changes over time. The early data show a jump in Medicaid and CHIP determinations since open enrollment began relative to recent enrollment trends; however, it is not possible to disaggregate how much of this growth is directly attributable to the ACA. Future CMS data will show how many individuals are newly eligible for coverage as states start to submit claims to access the enhanced federal matching dollars tied to this coverage. However, it will be very difficult to disentangle how much of the overall increased enrollment can be tied to the ACA requirements to streamline Medicaid eligibility and enrollment policies and coordination across health coverage programs that must be implemented in all states regardless of whether they implement the Medicaid expansion.
Endnotes
Kaiser Family Foundation, “Status of State Action on the Medicaid Expansion Decision, 2014,” available at https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/, accessed January 27, 2014.
Congressional Budget Office, “CBO’s May 2013 Estimate of the Effects of the Affordable Care Act on Health Insurance Coverage,” Table 1.
Rudowitz, R., “A Closer Look at the Uninsured Eligible for Medicaid,” Kaiser Commission on Medicaid and the Uninsured, The Henry J. Kaiser Family Foundation, December 20, 2013, available at: https://www.kff.org/health-reform/issue-brief/a-closer-look-at-the-uninsured-eligible-for-medicaid/.
Centers for Medicare and Medicaid Services, “Medicaid & CHIP: December Monthly Applications and Eligibility Determinations Report, January 22, 2014, available at http://medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/December-2013-Enrollment-Report.pdf.
Centers for Medicare and Medicaid Services, October-December 2013 Monthly Application and Eligibility Reports, available at http://medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/medicaid-moving-forward-2014.html
Department of Health and Human Services, “Health Insurance Marketplace: January Enrollment Report, for the period: October 1, 2013-December 28, 2013,” January 13, 2014, available at http://aspe.hhs.gov/health/reports/2014/MarketPlaceEnrollment/Jan2014/ib_2014jan_enrollment.pdf.
Centers for Medicare and Medicaid Services, October-December 2013 Monthly Application and Eligibility Reports, op cit.
Department of Health and Human Services, op cit.
“Key Lessons from Medicaid and CHIP for Outreach and Enrollment Under the Affordable Care Act,” Kaiser Commission on Medicaid and the Uninsured, The Henry J. Kaiser Family Foundation, June 2013. https://www.kff.org/medicaid/issue-brief/key-lessons-from-medicaid-and-chip-for-outreach-and-enrollment-under-the-affordable-care-act/ and Heberlein, M., Brooks, T., Alker, J., Artiga, S., and Stephens, J., “Getting into Gear for 2014: Findings From a 50-State Survey of Eligibility, Enrollment, Renewal and Cost-Sharing Policies in Medicaid and CHIP, 2012-2013” Kaiser Commission on Medicaid and the Uninsured, The Henry J. Kaiser Family Foundation, January 2013. https://www.kff.org/medicaid/report/getting-into-gear-for-2014-findings-from-a-50-state-survey-of-eligibility-enrollment-renewal-and-cost-sharing-policies-in-medicaid-and-chip-2012-2013/
Wachino, V. et al, “An Introduction to Medicaid and CHIP Eligibility and Enrollment Performance Measures, Kaiser Commission on Medicaid and the Uninsured, The Henry J. Kaiser Family Foundation, January 8, 2014, available at: https://www.kff.org/medicaid/issue-brief/an-introduction-to-medicaid-and-chip-eligibility-and-enrollment-performance-measures/.
Kaiser Commission on Medicaid and the Uninsured, Medicaid Enrollment: June 2013 Data Snapshot, (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, January 2014,) www.kff.org/medicaid/issue-brief/medicaid-enrollment-june-2013-data-snapshot.
Kaiser Commission on Medicaid and the Uninsured, CHIP Enrollment: June 2013 Data Snapshot. Kaiser Commission on Medicaid and the Uninsured, January 2014. www.kff.org/medicaid/issue-brief/chip-enrollment-june-2013-data-snapshot.
Ibid.